If you live with Crohn’s, you already know that life can feel like a rollercoaster with surprise loops. The link between stress and Crohn’s disease is real, and it can influence symptoms, mood, and day to day energy. When stress climbs, the gut often follows. The good news, small shifts can take the edge off and help you feel more in charge.
From Misdiagnosis to Understanding Stress and Crohn’s Disease
Before I had a clear diagnosis, I spent months collecting half answers and a pile of peppermint tea. Stress kept being blamed, while my symptoms kept getting louder. It took a second opinion to confirm Crohn’s disease. Stress was not the cause, but it did act like fuel on a smouldering fire. Knowing that changed how I planned my days and asked for help.
How Stress Affects Digestive Health and Crohn’s Symptoms
Stress can feel like someone pressing the fire alarm in your gut. In Crohn’s, it may fan inflammation and make symptoms more noticeable. People often ask does stress affect Crohn’s disease. Short answer, it can make symptoms worse, and a calmer day can sometimes feel kinder on the gut.
Research links higher stress with increased intestinal inflammation. Stress also nudges the immune system and can alter gut motility and sensitivity. That is why a tense week sometimes shows up as cramping, urgency, or fatigue.
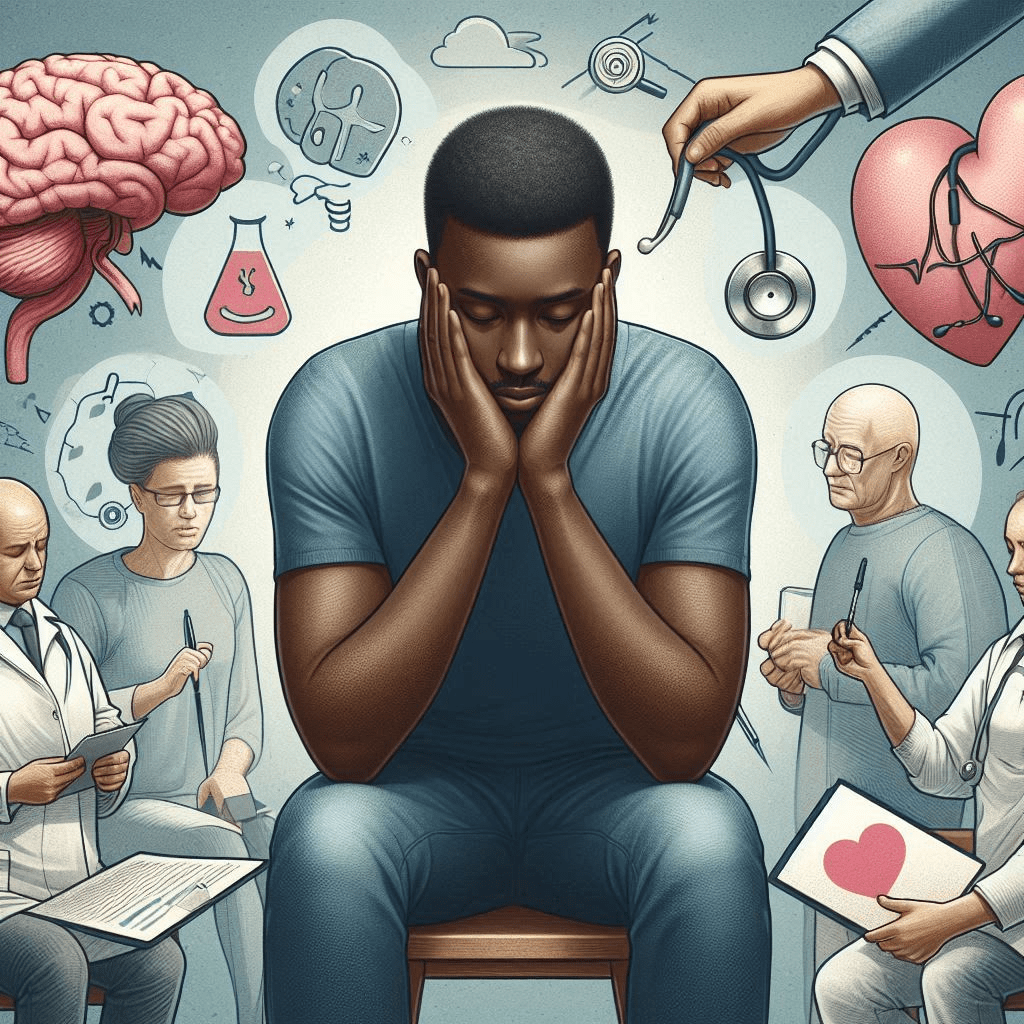
The Science of Stress and Gut Health
Your gut and brain are on a group chat called the gut brain axis. When stress spikes, your body releases cortisol, a stress hormone that can influence intestinal inflammation and the immune system. The microbiome can also shift with ongoing stress, which may affect digestive health and mood.
It is not only chemistry. Stress can lead to skipped meals, poor sleep, and less follow through on meds or appointments. That mix can set the stage for a stress-induced Crohn’s flare-up. This is why stress management for Crohn’s disease is worth treating as a daily habit, not a luxury.
Common Crohn’s disease stress triggers
- Last minute changes at work or school, especially without bathroom access.
- Short sleep and irregular meals, both can unsettle the gut.
- Conflict, big decisions, and money worries.
- New symptoms or fear of a flare, uncertainty is stressful on its own.
Small Wins for Stress Reduction
Managing stress can sound like another job. Instead, think small wins to reduce stress, the pocket sized actions you can actually do on a busy day.
- Take a micro break. Step outside for 5 minutes. Look at something far away. It helps reset your nervous system.
- Use a worry window. Park worries for later, then give them 10 minutes on paper. Your brain likes a queue.
- Talk it out. A quick chat with a friend, or your support network, can lower the temperature fast.
- Keep a symptom diary for patterns. Note food, sleep, stress, and symptoms. It makes triggers easier to spot and discuss.
Practical Tips for Managing Stress with Crohn’s Disease
- Mindfulness for Crohn’s disease. Treat your mind like a cluttered desk and tidy a corner. Try 5 to 10 minutes of attention on the breath or sounds around you. Aim for most days, not perfection.
- Deep breathing for stress relief. Sit, drop your shoulders, inhale through the nose for 4, exhale through the mouth for 6. Two minutes can help calm the body.
- Regular movement. Gentle exercise supports exercise and mood. Walking, yoga, or swimming can be easier on the gut. Start small and build.
- Sleep hygiene for Crohn’s. Keep a steady sleep and wake time, dim screens at night, and keep your bedroom cool and quiet. Better sleep often means better stress tolerance.
- Food and fluid. On tough days, think simple and regular. A healthy diet and gut health go hand in hand, but do not overhaul your eating during a flare without advice.
- Plan the practical. Pack meds, snacks, and a toilet card if that helps. Reducing uncertainty reduces stress.
- Know the myths. Many wonder can stress cause Crohn’s disease. It does not cause the condition, but stress can aggravate Crohn’s disease symptoms.
Stress and Crohn’s disease what we know
Stress management for Crohn’s disease is about stacking small habits. The aim is not zero stress, it is steadier days. The gut brain axis and Crohn’s are connected, and your choices can shift that balance in your favour. If you are thinking about how to manage Crohn’s disease during a busy week, start with one simple change you can keep.
No. Stress does not cause Crohn’s, but it can worsen symptoms and contribute to flare-ups. Managing stress supports your overall care.
Stress can raise cortisol, unsettle the immune system, and increase intestinal sensitivity. This may mean more pain, urgency, or fatigue.
Poor sleep, irregular meals, time pressure, and conflict are frequent triggers. A symptom diary can help identify your patterns.
Rest, gentle breathing, and simple meals may help you cope. Contact your care team if symptoms escalate or do not settle.
Mindfulness, deep breathing, light exercise, steady sleep, and planning ahead are useful. Try small steps you can keep up.
Avoid big changes without advice. Keep meals regular and simple, and speak to your doctor or dietitian for personalised guidance.
Living with Crohn’s is easier with clear information, practical tools, and people in your corner. Build routines that support you on average days, so you have more room when hard days arrive.
FAQs About Stress and Crohn’s Disease
Medical disclaimer. This blog post is for information only and is not medical advice. Always speak to your doctor about your situation and treatment. Do not start or stop medicines without your doctor’s guidance. Do not change your diet without advice from your doctor or a qualified healthcare professional.