Ever feel like your digestive system has gone rogue, running a one-person protest against dinner? Persistent abdominal pain, chronic diarrhoea, and fatigue might not just be a bad takeaway. They could be the first clues of Crohn’s disease symptoms. These signs often sneak in quietly before taking centre stage, leaving you wondering if your gut has joined the opposition. Understanding them isn’t about memorising medical jargon, it’s about regaining a sense of control over your body.
The thing about Crohn’s disease symptoms is that they refuse to follow a script. One person gets cramps and exhaustion, another spends half the day negotiating with the toilet. Think of it as a choose-your-own-adventure book written by a mischievous immune system.
Recognising the Signs of Crohn’s Disease
Crohn’s disease belongs to a troublesome family called inflammatory bowel diseases, where the immune system acts like an overzealous security guard attacking everything, including the furniture. The result is chronic inflammation anywhere from your mouth to your rear exit, though it usually sets up camp in the small intestine or colon.
Despite its unpredictability, there are tell-tale patterns worth noticing, like your gut sending smoke signals. These Crohn’s disease symptoms can range from mild annoyances to full-scale revolts.
Recognising a Flare-Up Before It Takes Over
A flare-up is your gut’s version of a fire drill, only nobody’s laughing. The inflammation ramps up, symptoms intensify, and your body reminds you who’s really in charge. Key Crohn’s flare-up symptoms include:
- Sharp or persistent abdominal pain
- Frequent and urgent diarrhoea
- Fatigue that laughs in the face of coffee
- Weight loss without the gym membership
- Low-grade fever or occasional rectal bleeding
When you spot these early, you can act before your body does its next magic trick, turning lunch into regret.
Early Signs of Crohn’s Disease
Before a full-blown flare-up, early signs of Crohn’s disease can be easy to dismiss. Slight abdominal discomfort here, a dodgy appetite there. Many chalk it up to stress, bad food, or an unsympathetic boss. But these early tremors matter. Catching them early can mean the difference between living with Crohn’s and Crohn’s running the show.
Look out for:
- Persistent lower-right abdominal pain
- Mild but regular diarrhoea
- Mouth ulcers that feel like paper cuts of betrayal
- Unexplained fatigue or weight loss
What Does Crohn’s Pain Feel Like
Describing Crohn’s pain is like trying to explain jazz. Everyone’s experience is different, but you know it when you feel it. Some people get stabbing cramps, others a dull ache that hums all day. Pain often shifts with the inflammation, proving that Crohn’s doesn’t believe in consistency.
Lesser-Known Crohn’s Disease Symptoms
Crohn’s may start in the gut, but it’s an overachiever. It likes to leave calling cards elsewhere too. These extraintestinal Crohn’s symptoms can make diagnosis tricky:
- Joint pain or stiffness, especially in the knees or hips
- Skin issues like red nodules or ulcers
- Eye inflammation causing pain or blurred vision
- Mouth ulcers that appear out of nowhere
In short, Crohn’s sometimes behaves like an unreliable roommate, causing chaos in every room.
Crohn’s Disease Complications and Diagnosis
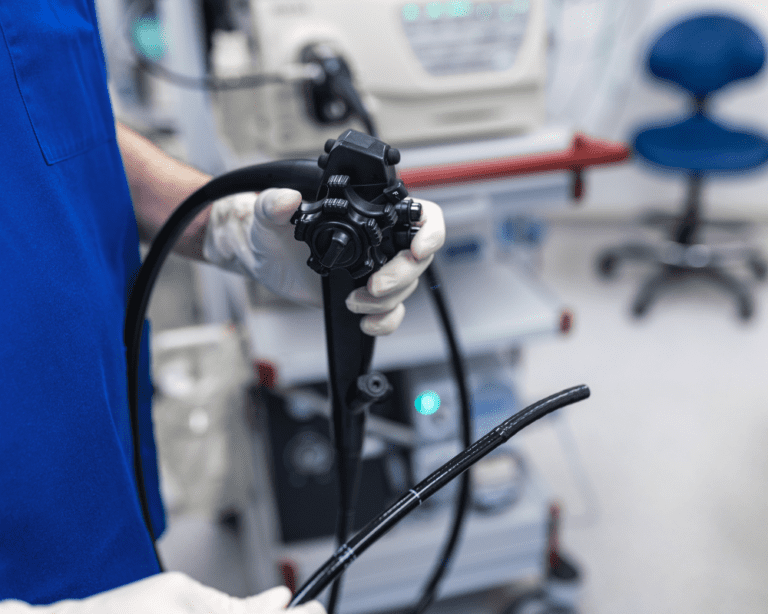
Diagnosing Crohn’s is a bit like detective work with fewer trench coats. Doctors look for patterns across symptoms, tests, and scans. Common steps include:
- Blood tests for inflammation and anaemia
- Stool tests to rule out infections
- Imaging (MRI or CT) to spot inflamed areas
- Endoscopy to see what your intestines have been hiding
It’s also worth distinguishing Crohn’s disease vs IBS symptoms. IBS may ruin your day, but Crohn’s tries to ruin your week.
Managing Crohn’s Disease Symptoms
No magic cure, but plenty of good strategies. Managing Crohn’s disease symptoms is less about fighting your body and more about negotiating with it. Medication helps calm the immune system’s overreaction, while lifestyle choices can tip the odds in your favour.
Small Adjustments, Big Difference
Here’s where behavioural science lends a hand. Humans, oddly enough, are more motivated by progress than perfection. Managing Crohn’s isn’t a test of willpower, it’s a masterclass in noticing feedback loops.
Take diet, for instance. People often frame food in moral terms, good or bad. A better approach is detective work. Which foods make you feel better, and which leave you regretting life choices? Keep a log, but think like a curious scientist, not a disappointed parent.
Then there’s stress. You can’t remove it, but you can redesign it. Rituals like breathing exercises, brief walks, or even tidy desks can send your body subtle cues of control. Think of it as training your nervous system to stop pressing the panic button every time your gut grumbles.
And never underestimate small victories. Taking your medication consistently, sleeping properly, or setting boundaries at work all reduce cumulative load, the same principle airlines use when shaving grams off meal trays. Small changes scale.
Lastly, mindset matters. Viewing Crohn’s as a conversation rather than a conflict changes everything. The aim isn’t to beat it but to out-negotiate it, turning your daily routines into quiet acts of self-defence.
Living With Crohn’s Day to Day
Crohn’s can be frustrating, exhausting, and occasionally absurd. But it also teaches you a kind of hyper-awareness, knowing your body’s patterns, energy levels, and triggers better than most athletes. Treat that knowledge like a superpower. Plan meals like a strategist, rest without guilt, and keep humour close by, it’s the cheapest medicine available.
In Summary
Understanding Crohn’s disease symptoms is the first step to living with confidence instead of confusion. This isn’t about perfection. It’s about progress, adaptation, and knowing that even a misbehaving gut can coexist with a well-lived life.
FAQs About Crohn’s Disease Symptoms
Early signs include mild abdominal pain, fatigue, diarrhoea, and mouth ulcers that come and go.
Early signs include mild abdominal pain, fatigue, diarrhoea, and mouth ulcers that come and go.
They often involve increased abdominal pain, urgency, exhaustion, and sometimes rectal bleeding or fever.
Stress doesn’t cause Crohn’s but can amplify flare-ups. Relaxation techniques and predictable routines help reduce stress-related triggers.
IBS causes discomfort without inflammation, while Crohn’s involves physical inflammation and sometimes bleeding.
Balanced diet, consistent sleep, and addressing anaemia or vitamin deficiencies can improve energy levels.