A Crohn’s disease colonoscopy can feel intimidating, even if it is routine. The worry is understandable, you are asked to empty your bowel, fast, then let a camera take a guided tour. The good news, with clear steps tailored to Crohn’s and the NHS way of doing things, you can reduce stress, protect your gut, and arrive feeling ready.
If you are reading this because you searched for colonoscopy Crohn’s, you are in good company. On the NHS, colonoscopy helps assess inflammation, guide treatment, and check healing. Knowing the plan, from colonoscopy preparation NHS instructions to what happens on the day, turns unknowns into a checklist you can actually use.
Crohn’s disease colonoscopy and how it helps
What is Crohn’s disease
Crohn’s disease is part of inflammatory bowel disease and it can cause persistent inflammation, pain, urgency and fatigue. This inflammation can affect any part of the digestive system, from the mouth to the anus, but most commonly involves the lower part of the small intestine (ileum) and the colon1. Symptoms can vary, and flare, but often include diarrhoea, abdominal cramps, weight loss and exhaustion.
What a Crohn’s colonoscopy shows
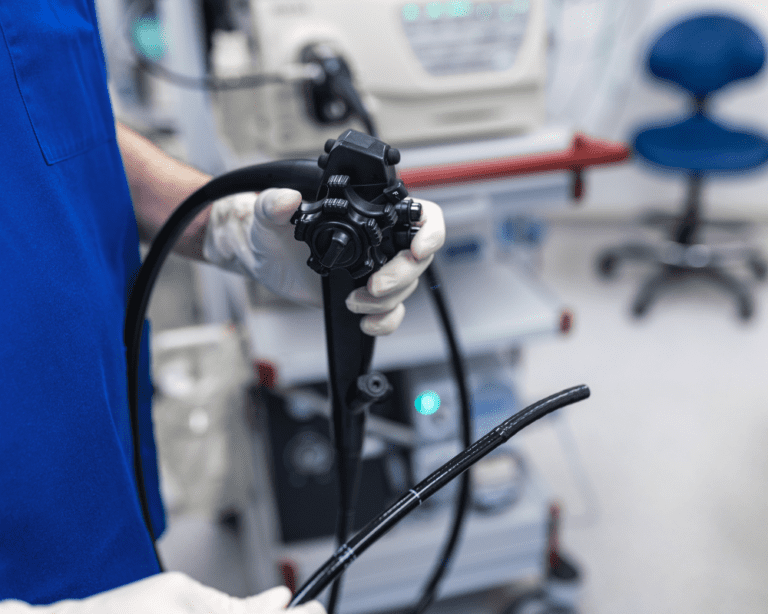
A colonoscopy gives your team a close look at the lining of the bowel, it can show ulcers, active inflammation, strictures and areas that look healed. During the test, a flexible tube with a camera, the colonoscope, is passed through the rectum. Small biopsies may be taken to check for microscopic changes, these are quick and usually painless.
What a scope can miss
No single test is perfect. Crohn’s can be patchy and sometimes sits higher up in the small bowel where the colonoscope cannot reach. That is why results are often combined with bloods, stool markers, MRI or CT scans to build a fuller picture.
Can a colonoscopy make Crohn’s worse
Most people only notice some wind, mild cramping or a day of feeling washed out. Serious problems like bleeding or a bowel perforation are rare. A flare after the test is uncommon, but talk to your team about your recent symptoms, medicines and any previous issues so they can plan safely for you.
My experience with Crohn’s colonoscopies on the NHS
NHS waiting lists can stretch patience. If things worsen while you wait, contact your IBD team or GP, they may adjust medicines or consider alternative checks such as calprotectin or imaging. There are also excellent support groups available through charities like Crohn’s and Colitis UK2 that can provide invaluable guidance and support.
What to expect from the colonoscopy camera
The camera is about finger width and the tube is flexible. You will usually be offered sedation and strong pain relief, some people choose gas and air. If you are searching “what to expect colonoscopy Crohn’s”, the short version is, you will change into a gown, a cannula may be placed, your team will monitor you, then the scope is gently guided in while images appear on a screen. Biopsies feel like little pinches, many people doze through.
Preparing for a colonoscopy on the NHS with Crohn’s
You cannot control everything, but these steps give you the best chance of a smooth day.
- Plan timing with your team. If possible, book during a steadier spell. If you are flaring, ask if the date should change.
- Share your full medication list. Include steroids, biologics, iron, blood thinners, painkillers and supplements. Ask about pauses or dose timing, especially around prep day.
- Follow the colonoscopy diet Crohn’s disease guidance. Most units advise lower fibre for a day or two, then a clear liquids diet the day before. Your letter will list what counts as clear, think water, squash without bits, clear soup, jelly without red or purple dyes.
- Hydrate like it is your job. Sip often to protect gut health and avoid dehydration, add oral rehydration salts if advised.
- Bowel cleansing matters. Your pack will include laxatives and instructions for colonoscopy bowel prep Crohn’s disease patients. Read it twice, set alarms, chill the solution, and use a straw. Barrier cream, soft wipes and comfy clothes help.
- Ask about sedation options. Tell the unit if scopes have been painful before, strictures or previous surgery can change the plan.
- Sort the practicals. Arrange a lift home, time off work, and a light plan for the day after.
What is the new NHS prep for colonoscopy
Many NHS bowel services now use split dosing, smaller volumes, or tablet regimens. Availability varies by hospital trust, ask your unit what they provide and what suits Crohn’s best for you.
- Low volume preps. Smaller drinks, sometimes with bisacodyl tablets.
- Split dose preps. Half the evening before, half on the day, often gives a cleaner result.
- Tablet based preps. Still limited in some areas, helpful if large drinks are hard to tolerate.
Talk to your IBD nurse or endoscopy unit about the options, and follow the specific NHS colonoscopy preparation you are given.

What a colonoscopy can detect
Colonoscopy checks more than Crohn’s.
- Ulcerative colitis. Inflammation in the colon lining.
- Colon cancer. An important screening and diagnostic test for higher risk groups.
- Polyps. These can be removed and sent for biopsy during the procedure.
- Diverticulitis. Inflamed pouches in the bowel wall.

After your colonoscopy what helps recovery
Rest, pass gas, eat small easy meals and keep sipping fluids. Mild cramps and spotting after biopsies can happen. If you feel unwell, feverish, or have ongoing heavy bleeding, follow the advice on your discharge sheet and contact the unit or NHS 111.
How often do you need a Crohn’s colonoscopy
There is no one schedule for Crohn’s disease colonoscopy frequency. It depends on your symptoms, previous findings, surgery history and cancer risk. Many people are checked every one to three years once things are stable, others need sooner reviews after a change in symptoms, for example an after-flare colonoscopy Crohn’s appointment. Ask your team what suits you right now.
Common questions about colonoscopies and Crohn’s
It shows the colon and end of the small bowel clearly, but Crohn’s can be patchy. Doctors combine scope findings with blood, stool and scans.
Most units advise lower fibre for a day or two, then a clear liquids diet the day before. Follow the instructions in your letter.
It is uncommon, but talk to your IBD team if you are flaring. They can advise on timing and prep type for you.
It usually starts the day before, sometimes split between evening and morning. Your hospital will give exact timings.
Most people get bloating or cramps that pass. Serious complications are rare, ask about your personal risk.
It varies with symptoms, history and risk. Many have one every one to three years once stable, ask your team.
Additional resources from the NHS
- NHS, colorectal cancer screening, https://www.nhs.uk/conditions/bowel-cancer-screening/
- NHS, Crohn’s disease information, https://www.nhs.uk/conditions/crohns-disease/
Important note
Remember, this article is for information only and is not medical advice. Always speak to your doctor about your situation and the right plan for you. Do not start or stop medicines without medical advice, and do not change your diet without guidance from your doctor or a healthcare professional.
Conclusion
A Crohn’s colonoscopy on the NHS is rarely anyone’s favourite day out, but it can be manageable. With clear prep, small practical tweaks and honest conversations with your team, you can get through it and get useful answers. If you want a quick recap, keep a list of colonoscopy tips Crohn’s patients swear by, hydrate, barrier cream, clear fridge, lift home, then rest.
- National Institute for Health and Care Excellence (NICE), https://www.nice.org.uk/guidance/ng129 ↩︎
- Crohn’s & Colitis UK, https://crohnsandcolitis.org.uk/ ↩︎