Stomach pain, sudden weight loss, relentless diarrhoea—if your gut feels like it’s throwing tantrums at random, you might be facing Crohn’s disease symptoms. Before you write it off as stress or “just a bug”, read this.
How Crohn’s Disease Symptoms Actually Show Up
Crohn’s disease symptoms can be as unique as a fingerprint. While some people experience a textbook presentation of the condition, others face a more ambiguous picture. The key is to recognise the early warning signs and seek medical advice to get a proper diagnosis and begin treatment. Here’s an overview of the range of symptoms associated with Crohn’s disease:
- Persistent Diarrhoea That Moves in Without Asking
- Loose, urgent, and showing up at the worst possible times—Crohn’s disease symptoms often begin here. And no, it’s not just last night’s takeaway.
- Abdominal pain and cramping
- When your gut starts protesting think of your intestines as a badly run call centre—overworked, understaffed, and ready to misfire at the slightest trigger. Crohn’s-related abdominal pain is usually crampy, nagging, and doesn’t play by digestive rules.
- Fatigue and Feeling Like You’re Coming Down With Something
- One of the most ignored Crohn’s disease symptoms. When you can’t keep your eyes open before lunch and everything feels like swimming through soup, it’s probably more than being ‘a bit tired’.
- Why You’re Eating Less and Losing Weight Without Trying
- If food has become more of a threat than a treat, you’re not alone. Inflammation, pain, and poor absorption tag-team your appetite—leaving your fridge full and your belt looser.
Most people assume pain equals severity. But habit‑forming bathroom fear can cause more daily damage than occasional flare‑ups. A behavioural economics twist: aversion to embarrassment often motivates better management than the pain itself.
Think of Crohn’s like a leaky boat. You patch one hole—say, diarrhoea—and another springs up, such as fatigue or mouth ulcers. That’s the illness behaving irrationally, and you learn fast which leak to plug first.
Remember: These are just some of the most common Crohn’s disease symptoms. The way they manifest and their severity can vary greatly from person to person.
What Does a Crohn’s Flare-Up Feel Like?
Think of a flare-up as your gut revving into a tantrum. The diarrhoea ramps up, the pain sharpens, and your patience wears dangerously thin. Crohn’s flare-up symptoms feel like a system crash—just with more bathroom visits. That’s what a flare-up can feel like. The intensity of the pain, the frequency of diarrhoea, and the overall feeling of unwellness can be significantly worse during a flare-up.
There’s no one-size-fits-all answer to how long a flare-up lasts or how often they occur. Some people experience them frequently, while others may have periods of remission with no symptoms at all. The important thing is to identify your triggers and work with your doctor to develop a management plan to minimise the impact of flare-ups on your life.
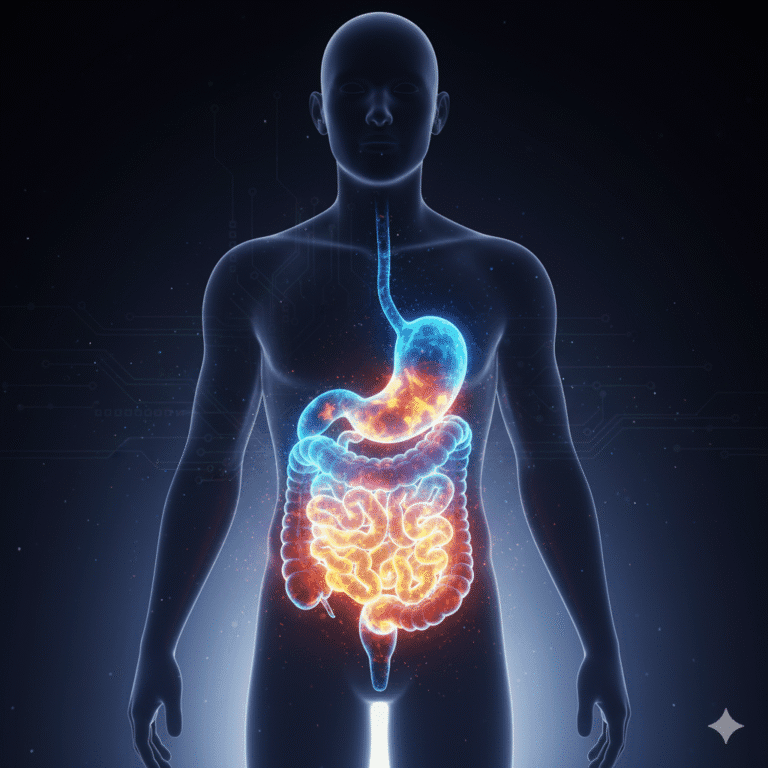
Where Does Crohn’s Usually Hurt?
Lower right pain? Could be your ileum acting up. Upper right? Maybe your jejunum’s jealous. The point is: Crohn’s disease symptoms don’t always stick to one postcode. Crohn’s disease can affect any part of your digestive system, from your mouth to your anus, but most commonly targets the small intestine and colon.
- Lower Right Abdominal Pain: This is a typical spot for Crohn’s-related pain, especially if the inflammation is focussed on the lower part of your small intestine (ileum) or your colon.
- Upper Abdominal Pain: Less common, but Crohn’s can also cause pain in the upper right abdomen if the inflammation is located in the upper part of your small intestine (jejunum).
- Other Areas of Discomfort: Remember, Crohn’s inflammation isn’t always confined to your gut. Joint pain, mouth ulcers, and skin problems can also be part of the picture.
It’s important to note: Pain location isn’t always an exact science. If you’re experiencing any kind of abdominal pain, especially alongside other Crohn’s symptoms, consult your doctor to get a proper diagnosis.
What Does Crohn’s Feel Like in the Beginning?
Most people shrug off the early Crohn’s disease symptoms as stress, dodgy takeaway, or a ‘bit of IBS’. But if you’re racking up sick days and buying more toilet roll than usual, it might be time for a rethink. Recognising these early warning signs can lead to a faster diagnosis and better disease management. Here are some common signs to watch out for:
- Persistent Diarrhoea: While everyone gets the occasional bout of diarrhoea, persistent, unexplained diarrhoea that lasts for weeks could be a sign of Crohn’s.
- Fatigue: Feeling constantly tired and lacking in energy can be a symptom of many conditions, but it’s also a common early sign of Crohn’s disease.
- Weight Loss: If you’re losing weight unintentionally, especially if you haven’t changed your diet or exercise routine, it could be a red flag for Crohn’s.
Don’t ignore these early signs! The sooner you get a diagnosis, the sooner you can start treatment and take control of your Crohn’s disease.
What Crohn’s Pain Actually Feels Like (Hint: It’s Not Just a Tummy Ache)
It’s not a polite gurgle. It’s a grudge. Crohn’s pain shows up as cramping, waves of discomfort, and a gut that acts like it’s auditioning for drama school. Antacids don’t help. Timing’s unpredictable. And the surrounding area often feels like it’s been through a boxing match. It’s a deep, crampy pain that can come and go in waves, often settling in the lower right abdomen but sometimes migrating to other areas. Unlike indigestion or heartburn, Crohn’s pain isn’t usually relieved by antacids. It can be a dull ache or a sharp, stabbing sensation, and the surrounding area may feel tender to the touch.
Here’s how Crohn’s pain differs from other types of gastrointestinal discomfort:
- Intensity: Crohn’s pain can be much more intense and persistent than indigestion or gas.
- Location: While indigestion often presents as a burning sensation in the upper abdomen, Crohn’s pain can be anywhere along your digestive tract.
- Accompanying Symptoms: Crohn’s pain is often accompanied by other symptoms like diarrhoea, fever, and fatigue, whereas isolated pain might point to a different cause.
Certain factors can worsen Crohn’s pain:
- Food intake: Spicy or greasy foods, processed food or those high in fibre, can sometimes trigger or exacerbate pain.
- Stress: Emotional stress can be a major trigger for Crohn’s flare-ups, and pain is often one of the first symptoms to worsen.
- Lack of sleep: When you’re well-rested, your body is better equipped to manage inflammation. Fatigue from sleep deprivation can worsen Crohn’s pain.
There are also ways to manage and alleviate Crohn’s pain:
- Medication: Anti-inflammatory drugs and steroids can help to reduce inflammation and ease pain.
- Heat therapy: Applying a heating pad or hot water bottle to your abdomen can provide soothing relief for cramps.
- Dietary changes: Identifying and avoiding your personal food triggers can significantly reduce pain.
- Stress management: Techniques like relaxation exercises and meditation can help you manage stress and minimise its impact on your Crohn’s symptoms.
Remember: Everyone experiences pain differently. If you’re concerned about your Crohn’s pain, talk to your doctor about the best management strategies for you.
What Does an Inflamed Bowel Feel Like?
Imagine your intestines as a traffic jam during a train strike. Inflammation acts like roadworks that never end—causing urgency, incomplete trips (if you catch my drift), and internal chaos. Welcome to one of the classic Crohn’s disease symptoms. Now picture roadblocks and potholes interrupting the flow of traffic. That’s what inflammation in the bowel feels like with Crohn’s disease.
The discomfort can manifest in several ways:
- Urgency and Frequency of Bowel Movements: Inflammation can irritate the lining of your intestines, triggering frequent and urgent bowel movements.
- Incomplete Bowel Movements: The inflammation can narrow the passage in your intestines, making it difficult to empty your bowels completely.
- Abdominal cramps and bloating: As your inflamed intestines struggle to process waste, you may experience cramping, bloating, and a general feeling of discomfort in your abdomen.
The severity of these sensations depends on the degree of inflammation and the location within your bowel.
Here’s how the level of inflammation can affect your experience:
- Mild Inflammation: You might experience occasional loose stools or mild cramping.
- Moderate Inflammation: Symptoms may become more frequent and intense, with urgency and incomplete bowel movements.
- Severe Inflammation: Constant pain, cramping, and severe diarrhoea can significantly impact your daily life.
Remember: Inflammation is a hallmark of Crohn’s disease. By understanding how it affects your bowels, you can better recognise and manage your crohn’s disease symptoms.
What Time of Day Is Crohn’s Pain Worse?
Some wake up feeling like they’ve swallowed barbed wire. Others feel fine—until they eat. Your Crohn’s disease symptoms may sync with circadian rhythm, food intake, or, let’s face it, life being inconvenient. Crohn’s pain can strike at any time, day or night. However, some people report experiencing worse pain:
- In the Morning: After a night’s rest, inflamed bowels might be stiffer and more irritated, leading to increased discomfort upon waking and throughout the morning.
- After Eating: Digestive activity can exacerbate pain, so some people experience a worsening of symptoms after meals, particularly those high in fibre or fat.
Here are some possible reasons for these patterns:
- Circadian Rhythm: Our bodies have natural cycles that influence inflammation levels. Certain inflammatory chemicals might fluctuate throughout the day, potentially causing pain to worsen at specific times.
- Food Intake and Digestion: The digestive process itself can irritate inflamed bowels. Pain might be more noticeable after meals as your digestive system works to break down food.
- Individual Variations: Everyone’s body is different, and the way Crohn’s manifests can vary greatly. Some people might have a specific time of day when their pain is worse, while others experience it more consistently.
Here’s what you can do to manage time-specific pain:
- Track your symptoms: Keeping a diary to record the timing and severity of your pain can help you identify patterns.
- Plan meals strategically: If you notice pain worsening after eating, try smaller, more frequent meals throughout the day. You can also discuss dietary modifications with your doctor to identify and avoid trigger foods.
- Talk to your doctor: If you’re experiencing significant pain at specific times of day, your doctor can help you adjust medications or lifestyle habits to minimise discomfort.
What Are the Early Warning Signs and Common Symptoms of Crohn’s Disease?
What Are the Early Warning Signs of Crohn’s?
Crohn’s disease can be a stealthy opponent, sometimes presenting with subtle signs that are easy to miss. However, being aware of these early warning signs can empower you to seek medical attention and get a timely diagnosis. Here’s what to watch out for:
- Persistent Diarrhoea: Diarrhoea That Won’t Quit. If it’s lasted longer than your last holiday, it’s probably worth a GP visit. Diarrhoea lasting for more than a few days, especially if accompanied by blood or mucus, could be a red flag.
- Changes in Bowel Habits: Unexplained constipation or a sudden change in your usual bowel pattern can be a sign of something amiss.
- Persistent Abdominal Pain: A dull ache or cramping pain in your abdomen, particularly in the lower right quadrant, that doesn’t go away could be an early indicator of Crohn’s.
- Unexplained Weight Loss: If you’re losing weight unintentionally, and it’s not due to diet or exercise changes, consult your doctor.
- Fatigue: The Tiredness You Can’t Sleep Off. It’s not laziness. It’s a body waging war inside your gut. One of the most ignored Crohn’s disease symptoms, and ironically, one of the most destructive. Feeling constantly tired and lacking in energy can be a symptom of many conditions, but it’s also worth mentioning to your doctor, especially if accompanied by other potential Crohn’s signs.
Remember: These are just some of the early warning signs. If you’re experiencing any of these symptoms persistently, don’t hesitate to schedule an appointment with your doctor to discuss your concerns.
What Are Common Symptoms of Crohn’s Disease?
- Chronic Diarrhoea: This is a hallmark symptom, often presenting as frequent, loose, and watery stools. It can be incredibly disruptive to daily life and leave you feeling drained.
- Abdominal Pain: A constant or recurring cramping pain in your abdomen, often in the lower right area, is another common symptom. The area may also feel tender to the touch.
- Fever and Fatigue: Crohn’s inflammation can cause a low-grade fever and leave you feeling constantly exhausted.
- Weight Loss and Loss of Appetite: Inflammation and digestive difficulties can make eating unpleasant, leading to a loss of appetite and subsequent weight loss.
- Rectal Bleeding: Blood in your stool can be a concerning symptom and warrants immediate medical attention.
- Mouth Ulcers: Painful sores in your mouth, although less common, can be a sign of Crohn’s disease.
- Perianal Disease: This refers to inflammation, irritation, or skin tags around the anus.
While these are the most common, it’s important to remember that Crohn’s disease can manifest in many ways. Don’t dismiss other symptoms you might be experiencing.
What Are the Characteristics of Crohn’s Disease?
Crohn’s disease goes beyond just a general feeling of unwellness. It can manifest in specific physical ways that offer clues to its presence. Here’s a breakdown of some characteristic features:
What Is Crohn’s Belly?
The term “Crohn’s belly” refers to the visible changes in the abdomen that can sometimes occur in people with Crohn’s disease. These changes can include:
- Bloating and Distension: Inflammation in the bowel can cause the abdomen to appear swollen and distended.
- Abdominal Masses: In some cases, inflammation can lead to the development of palpable lumps in the abdomen.
- Visible Bowel Loops: In severe cases, the inflamed sections of the intestines may become visible through the abdominal wall.
It’s important to note: Not everyone with Crohn’s disease will experience these changes. The severity and visibility of “Crohn’s belly” depend on the extent of inflammation and individual factors.
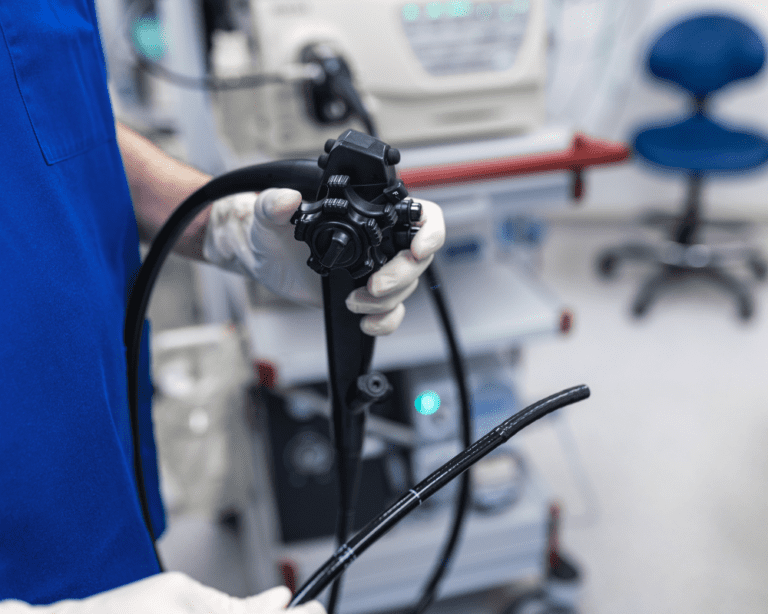
What Does Your Bowel Look Like with Crohn’s?
During an endoscopy or imaging test, doctors can see characteristic changes in the bowel of someone with Crohn’s disease. These changes include:
- Ulceration: The inflamed tissue in the bowel wall can develop deep, crater-like ulcers.
- Cobblestone Appearance: Inflammation can cause the lining of the bowel to thicken and develop a bumpy, cobblestone-like texture.
- Strictures: Chronic inflammation can lead to scar tissue formation, which can narrow the passage in the bowel (strictures).
- Fistulas: In some cases, deep ulcers can burrow through the bowel wall and create abnormal connections to other organs or the skin (fistulas).
By examining the appearance of the bowel, doctors can diagnose Crohn’s disease and determine the extent of the inflammation.
How Is Crohn’s Disease Diagnosed and Differentiated?
Diagnosing Crohn’s disease symptoms is like solving a whodunnit where all the suspects look guilty. You’ll need bloods, stool tests, scopes, and probably a small chat with your bowels via camera. Diagnosis often involves a combination of factors, including:
- Symptoms: A detailed discussion of your symptoms, including their duration, severity, and any accompanying signs.
- Medical History: Your doctor will inquire about your overall health, family history, and any medications you’re taking.
- Physical Examination: A physical exam to assess for abdominal tenderness, masses, or other signs.
- Blood Tests: While not diagnostic, blood tests can reveal signs of inflammation or anaemia, common in Crohn’s disease.
- Stool Tests: These tests can check for the presence of blood, white blood cells, or parasites in your stool, which might indicate inflammation or infection.
- Imaging Tests: X-rays, CT scans, or MRIs can help visualise your digestive tract and identify inflammation, strictures, or fistulas.
- Endoscopy: A procedure where a thin, flexible tube with a camera is inserted into your digestive tract to directly visualise the lining of the intestines and take biopsies (tissue samples) for further examination.
What Could Be Mistaken for Crohn’s?
Several conditions can share similar symptoms with Crohn’s disease, making diagnosis a bit trickier. Here are some common culprits:
- Ulcerative Colitis: This inflammatory bowel disease (IBD) affects only the inner lining of the colon and typically causes rectal bleeding and cramping in the lower left abdomen, unlike Crohn’s which can affect any part of the digestive tract.
- Irritable Bowel Syndrome (IBS): IBS is a functional bowel disorder that causes abdominal pain, cramping, bloating, and diarrhoea, but without the inflammation seen in Crohn’s. IBS sufferers also typically don’t experience weight loss, fever, or rectal bleeding.
- Microscopic Colitis: This condition causes chronic watery diarrhoea but without the visible inflammation seen in Crohn’s disease. Diagnosis often relies on stool tests and biopsies.
- Bacterial or Parasitic Infections: Certain infections can cause symptoms similar to Crohn’s, such as diarrhoea, abdominal pain, and fever. Stool tests can help differentiate these infections from Crohn’s disease.
Accurate diagnosis is crucial for receiving the proper treatment. Your doctor will carefully consider your symptoms, medical history, and test results to differentiate Crohn’s disease from other conditions.
How Does Crohn’s Disease Present and Progress Over Time?
Crohn’s disease can be unpredictable. Here’s a look at some aspects of its presentation and progression:
What Is Silent Crohn’s?
Silent Crohn’s disease refers to a situation where a person has the condition but experiences minimal or no symptoms. This can be frustrating as it delays diagnosis and treatment. Sometimes, silent Crohn’s is only discovered incidentally during imaging tests
What Are the Sneaky Symptoms of Crohn’s Disease?
Crohn’s disease can be a master of disguise. In addition to the more well-known symptoms, it can manifest in less obvious ways that can be easily dismissed. Here are some sneaky symptoms to watch out for:
- Joint Pain: Inflammation isn’t always confined to the gut. Crohn’s disease can cause pain, swelling, and stiffness in your joints, particularly the ankles, knees, and hips.
- Eye Inflammation: Conditions like uveitis (inflammation in the eye) or episcleritis (inflammation of the white of the eye) can be associated with Crohn’s disease.
- Skin Rashes: Certain skin rashes, like erythema nodosum (red, tender nodules) or pyoderma gangrenosum (painful ulcers), can be linked to Crohn’s disease.
- Delayed Growth and Development in Children: Crohn’s disease can affect nutrient absorption, leading to stunted growth and development in children.
- Nutritional Deficiencies: Due to inflammation and malabsorption, deficiencies in iron, vitamin B12, and other essential nutrients can occur.
- Mouth Ulcers: As mentioned earlier, painful sores in your mouth can be a sign of Crohn’s disease, although not as common as other symptoms.
Being aware of these atypical symptoms can help you recognise a broader picture of Crohn’s disease and seek medical evaluation if needed.
What Bowel Symptoms Should Not Be Ignored?
While some bowel issues might seem like a passing nuisance, certain symptoms warrant immediate medical attention, especially if they persist:
- Severe or Bloody Diarrhoea: Especially if accompanied by dehydration or dizziness.
- Persistent Abdominal Pain: Unrelenting pain that disrupts your daily activities or sleep is a cause for concern.
- High Fever: A fever, particularly alongside other symptoms, could indicate a complication like an abscess.
- Vomiting: Persistent vomiting can lead to dehydration and electrolyte imbalance.
- Inability to Pass Stool or Gas: This could be a sign of a blockage in your intestines.
Don’t hesitate to seek medical attention if you experience any of these concerning bowel symptoms. Early diagnosis and treatment can significantly improve your quality of life.
Is Crohn’s on the Right or Left?
There’s no single answer to this. Crohn’s disease can affect any part of your digestive tract, from the mouth to the anus. However, it most commonly targets the lower part of the small intestine (ileum) and the colon.
- Right-Sided Pain: Pain localised in the lower right abdomen often suggests inflammation in the terminal ileum, a common site for Crohn’s involvement.
- Left-Sided Pain: Pain on the left side might indicate involvement of the descending colon or sigmoid colon.
- Pelvic Pain: In some cases, Crohn’s can affect the small bowel close to the rectum, causing pain in the pelvic region.
Remember: Location of pain is just one piece of the puzzle. A thorough evaluation by your doctor is essential for accurate diagnosis.
Do People with Crohn’s Get Sick a Lot?
People with Crohn’s disease may be more susceptible to certain infections due to:
- Suppressed Immune System: Medications used to treat Crohn’s disease can sometimes dampen the immune system, making you more vulnerable to infections.
- Malnutrition: Nutrient deficiencies caused by Crohn’s can weaken your immune response.
- Disrupted Gut Microbiome: The healthy bacteria in your gut play a vital role in immunity. Inflammation in Crohn’s can disrupt this delicate balance, increasing susceptibility to infections.
Here’s how to reduce your risk of infections:
- Vaccinations: Stay up-to-date on recommended vaccinations to protect yourself from preventable illnesses.
- Frequent Handwashing: This simple practice can significantly reduce the spread of germs.
- Hygiene: Maintain good hygiene practices to minimise exposure to potential pathogens.
- Maintain a Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can support your immune system.
- Open Communication with Doctor: Discuss any concerns about infections with your doctor, who can advise on appropriate preventative measures.
Do People with Crohn’s Have Diarrhoea Every Day?
The frequency and severity of diarrhoea in Crohn’s disease can vary greatly from person to person. Here are some factors that influence your experience:
- Disease Activity: During flare-ups, diarrhoea is likely to be more frequent and severe.
- Location of Inflammation: Inflammation closer to the rectum can cause more frequent loose stools compared to inflammation higher up in the digestive tract.
- Dietary Triggers: Certain foods or ingredients can worsen diarrhoea in some people with Crohn’s. Identifying and avoiding these triggers can help manage symptoms.
- Medications: Some medications used to treat Crohn’s disease can have side effects like diarrhoea.
Here’s what to expect:
- Chronic Diarrhoea: This is a hallmark symptom of Crohn’s disease, but it doesn’t necessarily have to be an everyday occurrence. Some people experience periods of remission with minimal or no diarrhoea.
- Flare-Up Diarrhoea: During flare-ups, diarrhoea can become more frequent and severe.
- Managing Diarrhoea: While there’s no guaranteed cure for Crohn’s-related diarrhoea, lifestyle modifications, dietary adjustments, and medication can significantly improve your experience. Talking openly with your doctor is key to developing a management plan that works for you.
Living with Crohn’s Disease: Hope and Empowerment
Crohn’s disease can be a challenging companion, but it doesn’t have to define you. With knowledge, self-care, and the right support system, you can manage your condition and live a fulfilling life. Here are some tips:
- Build a Strong Support System: Surround yourself with people who understand your condition and offer emotional support.
- Educate Yourself: The more you know about Crohn’s disease, the better equipped you are to manage it.
- Find a Doctor You Trust: Having a doctor who listens to your concerns and works collaboratively with you on your treatment plan is crucial.
- Maintain a Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can help nourish your body and manage symptoms.
- Identify and Avoid Food Triggers: Pay attention to how certain foods affect your symptoms and make adjustments to your diet accordingly.
- Manage Stress: Stress can exacerbate Crohn’s symptoms. Explore relaxation techniques like yoga or meditation to manage stress effectively.
- Don’t Be Afraid to Ask for Help: Living with a chronic illness can be overwhelming. Don’t hesitate to seek help from therapists, social workers, or support groups.
- Stay Positive: Maintaining a positive outlook can significantly improve your quality of life. Focus on the things you can control and celebrate your victories, no matter how small.
Remember, you’re not alone on this journey. With the right tools and resources, you can manage your Crohn’s disease and live a life full of possibilities.
Beyond the Physical: Addressing the Emotional Impact of Crohn’s Disease
Crohn’s disease isn’t just a physical challenge; it can take a toll on your emotional well-being too. Here’s how to navigate the emotional rollercoaster and protect your mental health:
- Coping with Uncertainty: The unpredictable nature of Crohn’s, with its flares and remissions, can be emotionally draining. Finding healthy coping mechanisms like journaling or mindfulness exercises can help you manage the uncertainty.
- Body Image Issues: Chronic illness can affect your body image. Focus on what your body can do, celebrate your strength and resilience, and surround yourself with supportive people who value you for who you are.
- Social Isolation: The fear of unpredictable symptoms or bathroom urgency can lead to social isolation. Don’t be afraid to explain your condition to friends and family. You might be surprised by the understanding and support you receive. There are also online communities and support groups specifically for people with Crohn’s disease where you can connect with others who understand your experiences.
- Feeling Frustrated and Angry: It’s perfectly normal to feel frustrated or angry with your condition. Talk to a therapist or counsellor to develop healthy ways to express and manage these emotions.
- Depression and Anxiety: Chronic illness can increase your risk of depression and anxiety. If you’re experiencing persistent feelings of sadness, hopelessness, or worry, don’t hesitate to seek professional help. Remember, there’s no shame in asking for support for your mental health.
The Future of Crohn’s Disease: Research and Hope
While there’s currently no cure for Crohn’s disease, researchers are actively exploring new avenues for treatment and management. Here’s a glimpse into what the future might hold:
- Personalised Medicine: This approach tailors treatment plans to the specific characteristics of your Crohn’s disease, maximising effectiveness and minimising side effects.
- Advanced Diagnostics: More accurate and non-invasive diagnostic tools are being developed to enable earlier diagnosis and more targeted treatment strategies.
- Dietary and Nutritional Therapies: Research is ongoing into the role of diet and gut microbiome in managing Crohn’s disease. This could lead to personalized dietary plans and the development of prebiotics and probiotics to promote gut health.
- Promising New Medications: Researchers are exploring new drug therapies that target specific inflammatory pathways in Crohn’s disease, potentially leading to more effective and long-lasting symptom control.
- Stem Cell Therapy: While still in its early stages, stem cell therapy holds promise for repairing damaged tissue in the gut and potentially achieving remission in Crohn’s disease.
FAQs about Crohn’s Symptoms
Common symptoms of Crohn’s Disease include persistent and frequent diarrhoea, crampy abdominal pain, fever, loss of appetite, weight loss, fatigue, and rectal bleeding. These symptoms can vary in severity and may come and go over time.
Crohn’s-related abdominal pain is often accompanied by other symptoms such as diarrhoea, fever, and weight loss. It may also feel more crampy and persistent, with the gut feeling sore to the touch. If you’re experiencing abdominal pain along with other symptoms associated with Crohn’s Disease, it’s important to consult a healthcare professional for further evaluation and diagnosis.
In addition to the more common symptoms, Crohn’s Disease can also manifest in less obvious ways, such as mouth ulcers, joint pain, eye inflammation, and skin rashes. It can also lead to ulcer tracts in the intestines that may tunnel into adjacent organs, causing infections. Being aware of these lesser-known symptoms can help you recognise the signs of Crohn’s Disease and seek timely medical intervention.
Conclusion: Living a Fulfilling Life with Crohn’s Disease
Crohn’s disease may be a part of your life, but it doesn’t have to control it. By taking charge of your health, advocating for yourself, and building a strong support system, you can manage your symptoms and live a life brimming with purpose and joy. Remember, you are more than your diagnosis. With knowledge, self-care, and a positive outlook, you can embrace all that life has to offer.