Crohn’s disease in children can feel overwhelming at first. The symptoms are confusing, the internet is noisy, and school does not pause for clinic days. This guide gives you clear, practical steps on symptoms, diagnosis, and managing daily life, so your family can move from firefighting to feeling prepared.
What Is Crohn’s Disease in Children
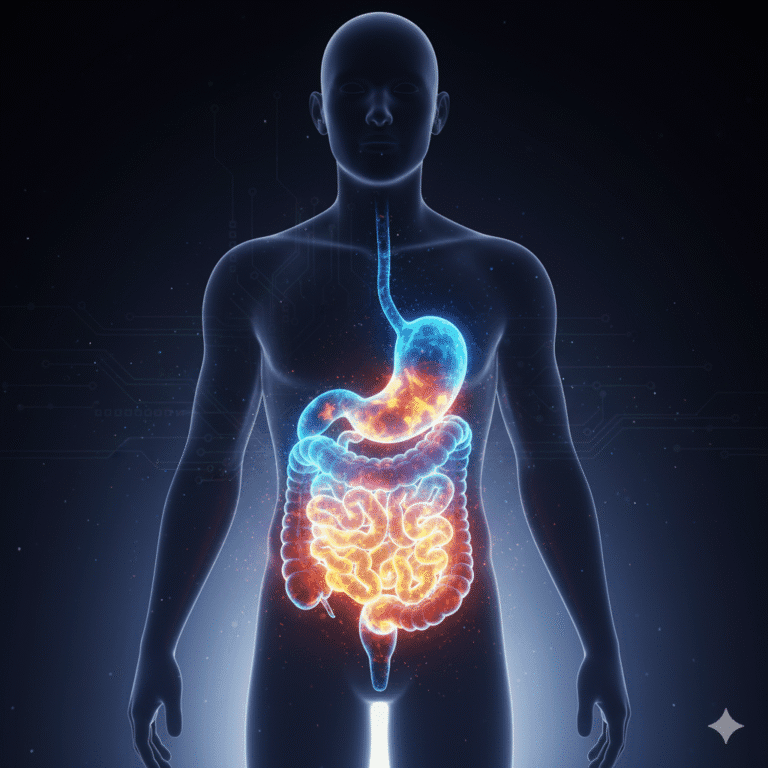
Crohn’s disease is an inflammatory bowel disease, often called IBD. It causes ongoing bowel inflammation, most often in the small intestine or colon, which can lead to tummy pain, diarrhoea, weight loss, and tiredness. A paediatric gastroenterologist leads care for children. You may also see the term pediatric Crohn’s disease in US-based resources.
Symptoms of Crohn’s Disease in Children
Symptoms vary from child to child, and they can come and go. Common signs include:
- Abdominal pain or cramping, often after eating
- Diarrhoea, sometimes with urgency
- Unintended weight loss or poor appetite
- Fatigue and low energy
- Slow growth or delayed puberty
- Mouth ulcers or perianal pain
- Iron deficiency or low vitamin levels
If these patterns persist, keep notes and speak to your GP for advice. Early signs of Crohn’s disease in children can be subtle, so tracking small changes helps.
Surprising Links and Practical Truths
Research hints at interesting connections. Some studies suggest oral bacteria may influence gut inflammation, so good dental care supports overall health, even if it does not treat Crohn’s directly. Children raised around animals sometimes show lower IBD rates in research, though mud is not medicine. What consistently helps is a plan, steady routines, and a strong support system.
Treatment may include medicines, nutritional therapies, and sometimes surgery. Dietary management can be useful during flares or growth spurts. The right mix depends on your child’s needs, goals, and what fits daily life.

Coping with Crohn’s Disease in Children Psychology and Practicality
Small, repeatable habits give children back a sense of control. Try family mealtimes where possible, regular check-ins, and visible progress markers. A food journal for Crohn’s can show patterns without guesswork. When a flare knocks confidence, reframe it as fresh information, not failure. You are building skills, one day at a time.
Explaining Crohn’s Disease to a Child
- Use simple, honest language. For example, Crohn’s means parts of the gut get sore and need help to heal.
- Link the condition to action, such as medicines, rest, and symptom tracking.
- Offer choices where safe, like which snack to try or which notebook to use.
- Practise short scripts for friends or teachers, so your child feels ready rather than put on the spot.
Managing Crohn’s Disease in Children Day to Day
- Create a school support plan with the SENCO or pastoral lead, covering toilets, lateness, and exam adjustments.
- Set a simple symptom tracking routine, using a one to ten scale for pain and energy.
- Keep medicines and a spare set of clothes in a small kit.
- Use dietary management with your clinical team, and note any triggers.
- Protect sleep and movement, short walks beat all or nothing plans.
- Build a strong support system of family, friends, school, and patient groups.
Early Signs, Diagnosis and Action
Parents often spot patterns before anyone else. Jot down symptoms of Crohn’s disease in children, meal notes, and school impacts. Photos of rashes or mouth ulcers can help too. Bring your notes to appointments so decisions are based on trends, not single days.
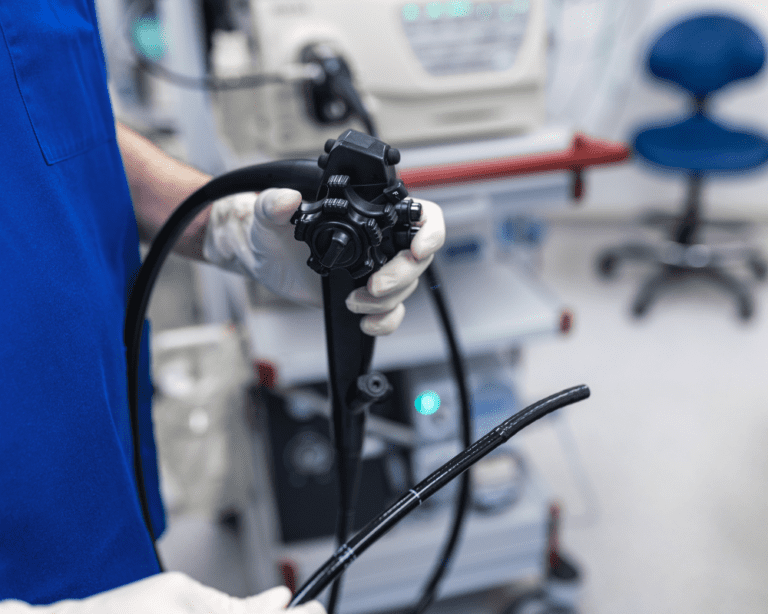
Crohn’s Disease Diagnosis in Children
Diagnosis usually combines medical history, examination, and tests. These may include blood tests for inflammation or nutrition, stool tests such as faecal calprotectin, imaging like MRI, and endoscopy to look directly at the gut. A paediatric gastroenterologist will guide the process and explain each step.
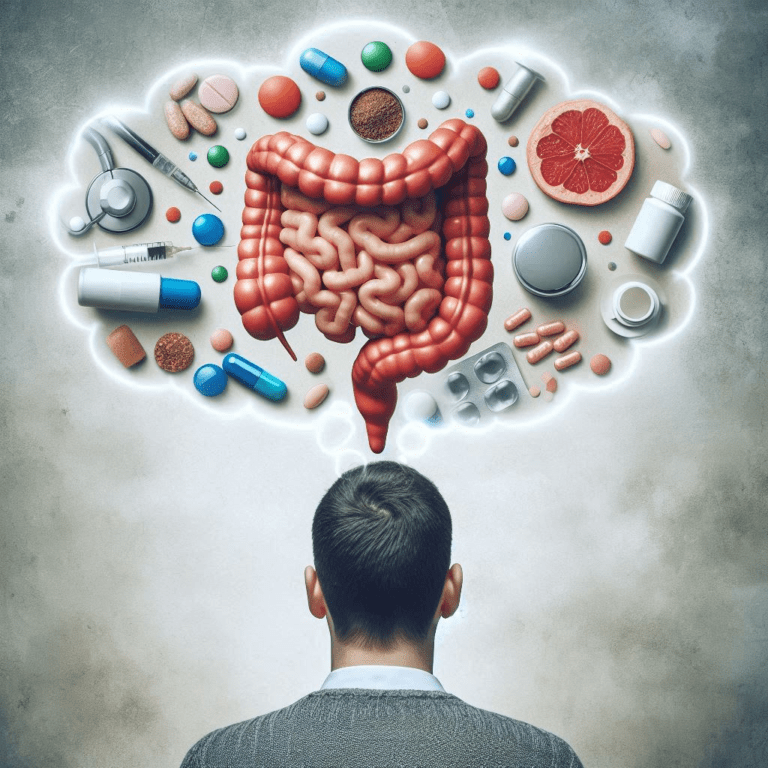
Treatment for Crohn’s Disease in Children
Treatment aims to calm inflammation, reduce symptoms, and support growth. Options can include nutritional therapy, for example exclusive enteral nutrition, anti inflammatory medicines, immune modulating drugs, biologics, and, if needed, surgery. Dietitians advise on dietary changes for paediatric Crohn’s disease during flares and recovery. Plans are reviewed regularly as children grow.
Medical information Remember, this blog post is intended for informational purposes only and should not be construed as medical advice. Always consult with your doctor to discuss your child’s situation and the best course of treatment. Do not start or stop medicines, and do not change diet, without speaking to your doctor or a healthcare professional.
Answers to Common Questions About Crohn’s Disease in Children
Tummy pain, diarrhoea, weight loss, and fatigue are common. Slow growth and mouth ulcers can appear too. Speak to your GP if patterns persist.
Doctors use history, blood and stool tests, scans, and endoscopy. A paediatric gastroenterologist explains each step and why it helps.
Diet can support symptom control and growth. Keep a food journal and ask a dietitian about dietary changes for pediatric Crohn’s disease.
Use simple words about sore gut and healing. Link it to medicines, rest, and symptom tracking. Practise short scripts for school.
Yes, it helps with toilets, lateness, and exams. Ask for a written school support plan and a key contact.
Options include nutritional therapy, medicines, and sometimes surgery. Plans change as children grow and needs shift.
Often yes with planning and rest breaks. Share their care needs with leaders and pack medicines and snacks.