Lost in the gastrointestinal maze, wondering if Crohn’s disease vs. ulcerative colitis is behind the mayhem? You’re not alone. Think of this as your treasure map, with a few behavioural detours to keep things interesting. Spoiler: no pop quiz, just practical insights to help you decode the chaos.
Crohn’s Disease vs. Ulcerative Colitis: Which Hits Harder?
Ah, the age-old question: which one’s worse? It’s like comparing apples and oranges, except neither is particularly sweet. Let’s break it down.
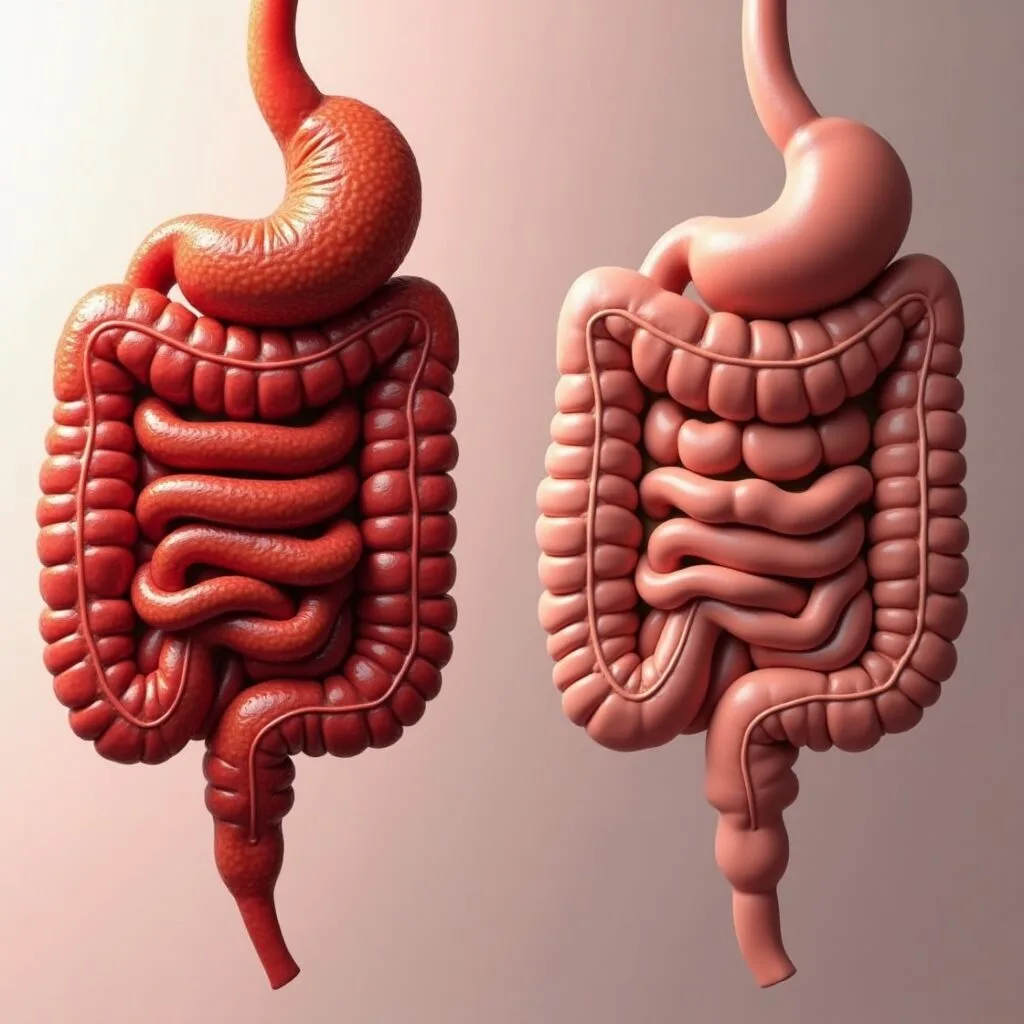
Crohn’s disease is the wildcard, targeting any part of your digestive tract from start to finish. Ulcerative colitis, however, stays rooted in the colon, refusing to roam elsewhere.
Severity can vary widely for both. Crohn’s might involve deeper layers of your gut wall, whereas Colitis often limits its wrath to the inner lining. To put it simply: one isn’t universally “worse” than the other; they’re just bad in their own unique ways.
“Both diseases are like two sides of the same coin,” remarks Dr. Jane Smith, a leading gastroenterologist. “They share many symptoms but have distinct characteristics that necessitate different treatment approaches.”
Crohn’s Disease vs. Ulcerative Colitis: Spotting the Signs
Your body’s always sending signals, though it’s less Shakespeare and more SOS. Overlaps like abdominal pain, diarrhoea, and fatigue might not just be from your late-night Netflix binge—your gut’s genuinely out of sorts.
Blood in your stool? That’s colitis raising its hand. Achy joints or irritated skin? Crohn’s is likely vying for attention. Both conditions love the spotlight, but their methods are as distinct as night and day.
But here’s a novel idea—have you considered stool tests? Yes, you heard right. A comprehensive stool analysis can provide invaluable data, like inflammation markers, that help doctors tell these two maladies apart. Don’t knock it until you’ve tried it!
Treatment Twists: One Size Doesn’t Fit All
Comparing treatments for Crohn’s and colitis is like comparing a hammer to a screwdriver. Both fix issues, but only when used in the right context. Mix them up, and you’ll have a bigger problem on your hands.
Medications such as anti-inflammatories and immunosuppressants are common combatants for both diseases. However, surgical approaches differ. Colitis might end with a colectomy—complete removal of the colon—while Crohn’s rarely calls for such a drastic measure.
An emerging option worth noting is fecal microbiota transplantation (FMT). Think of it as a neighbourhood renovation for your gut, where healthy bacteria move in to clean up the place. It’s unconventional, but promising.
Crohn’s Disease vs. Ulcerative Colitis: Modern Solutions to Old Gut Feuds
Managing these digestive dilemmas requires a targeted approach. Biologics, for example, act like precision snipers, targeting inflammatory proteins without collateral damage.
Dietary management often gets sidelined. It’s less about banning gluten or sugar and more about strategic choices. A food journal can be your investigative toolkit, identifying that seemingly harmless yoghurt as a prime suspect.
But here’s the twist: gut health isn’t just physical—it’s psychological. Chronic illness brings emotional baggage heavier than a holiday suitcase. Enter cognitive behavioural therapy (CBT), a proven strategy to reduce stress, improve sleep, and even lessen symptoms. Imagine CBT as the personal trainer for your mind, coaching you through the tough times with actionable strategies.
If we zoom out, we see treatments evolving toward precision medicine. Genetic testing and microbiome analysis now guide care, offering a bespoke approach. It’s less trial-and-error and more tailored problem-solving—a win for patients and clinicians alike.
Challenging Your Understanding: Mindful Eating
Let’s veer off the beaten track. Ever tried mindful eating? It’s not just for the yoga crowd. Being present and intentional with meals taps into the gut-brain connection and could help ease symptoms. Literal food for thought.
Wrapping It Up
Crohn’s and colitis are like siblings with wildly different temperaments. If you or someone you know is wrestling with symptoms, start with a clear diagnosis. And remember, these conditions don’t define you. You’re so much more than a diagnosis or a label.
There you have it—a digestible guide to the indigestible woes of Crohn’s and Colitis. Take this information, marinate on it, and consult your healthcare professional. Because when it comes to your health, you should be as assertive as a cat demanding breakfast at 5 a.m.
It’s crucial to remember one thing: always consult a healthcare professional for a proper diagnosis and treatment plan tailored to your needs. Even the most insightful articles and well-intentioned advice can’t replace the expertise of a medical doctor. When it comes to your health, consider this your friendly nudge to seek professional guidance. Trust me, Dr. Google doesn’t have a medical degree.
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus, and often involves all layers of the intestinal wall. Ulcerative colitis, on the other hand, is limited to the colon and rectum, affecting only the innermost lining. Both conditions cause inflammation, but their patterns and scope of impact differ significantly.
While there’s symptom overlap—like abdominal pain, diarrhoea, and fatigue—there are telltale signs. Blood in the stool is more common with ulcerative colitis, whereas Crohn’s disease often causes complications outside the gut, such as joint pain or skin issues. Stool tests and imaging studies can help pinpoint the cause.
Treatment options include anti-inflammatory medications, immunosuppressants, and biologics tailored to reduce inflammation. Surgery may be needed in severe cases—colectomy is more common in ulcerative colitis, while Crohn’s often involves removing narrowed or damaged sections of the digestive tract. Precision medicine is also making strides in treatment customisation.
Dietary adjustments can reduce symptoms, though they don’t replace medical treatment. Identifying trigger foods is key—spicy foods, dairy, and high-fibre items may aggravate symptoms. Food journaling is an effective way to monitor reactions. A low-FODMAP diet or nutritionist-guided plan may also help manage symptoms.
Living with a chronic illness like Crohn’s disease or ulcerative colitis can lead to stress, anxiety, or depression. Cognitive behavioural therapy (CBT) and mindfulness practices are proven to help manage these emotional challenges. Support groups and therapy can also provide valuable coping mechanisms.