One minute you’re demolishing a pepperoni pizza with all the grace of a Saturday-night Netflix binge — the next, your gut starts staging a protest louder than a toddler denied ice cream. That, my friend, is often how Crohn’s introduces itself. But behind those unruly symptoms lies a tale few know: the history of Crohn’s disease is a quirky, misdiagnosed, and occasionally misnamed saga that could rival most soap operas for plot twists. Let’s rewind the medical reel and revisit the history of Crohn’s disease, a tale that’s been as misdiagnosed as it’s misunderstood — and often ignored until it became too loud to dismiss.
How Did Crohn’s Disease First Appear in Medical Records
Long before Crohn’s made its red-carpet debut in the annals of medicine, it was skulking about in the background — misidentified, misinterpreted, and, frankly, misunderstood. Like a B-list actor finally getting their big break, Crohn’s lurked in the digestive wings until the 1930s.
In the early 1930s, during the Great Depression – when folks were already grappling with enough misery – a trio of doctors dropped a medical bombshell. Dr. Burrill B. Crohn (yep, the guy with the last name that rings a bell), Dr. Leon Ginzburg, and Dr. Gordon D. Oppenheimer teamed up to discover what we now know as Crohn’s disease.
How Crohn’s Disease Got Its Name and an Attitude
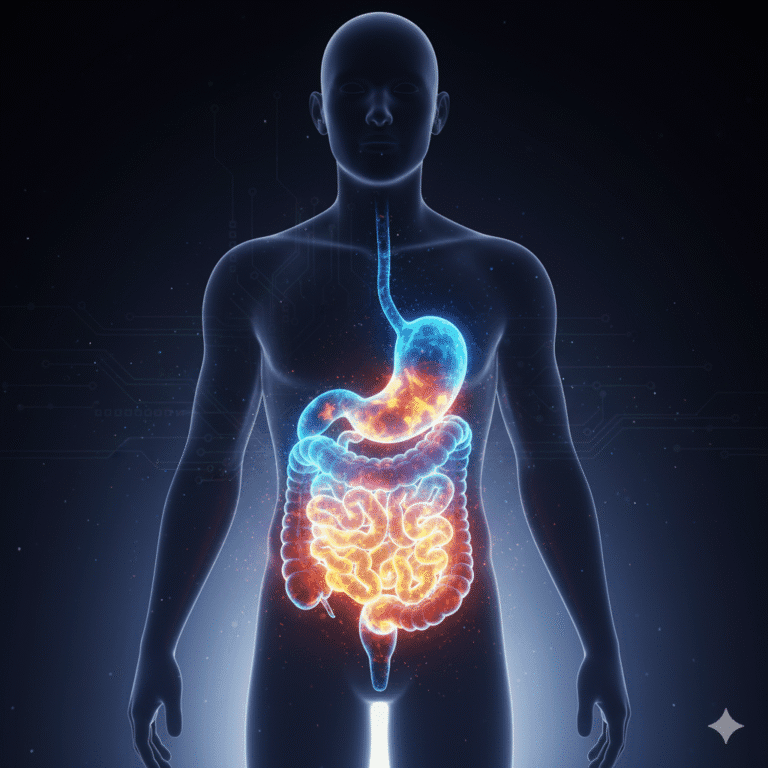
Picture your intestines throwing a sit-in during a dinner party — inflammation plonking itself at the head of the table, refusing to leave. That’s essentially what Crohn’s is: chronic, unwelcome, and oddly persistent. The name might sound like an old law firm, but the symptoms are anything but polite. Naming it was only part of the story — the history of Crohn’s disease is a messy mix of medical misfires, mistaken identities, and eventually, begrudging recognition.
As for the exact reason behind this digestive drama, well, that’s the tricky part. We’re still unraveling the mystery of what triggers Crohn’s, but it seems that both genetics and environmental factors join forces in this not-so-fantastic voyage.
Why Crohn’s Took Decades to Be Properly Diagnosed
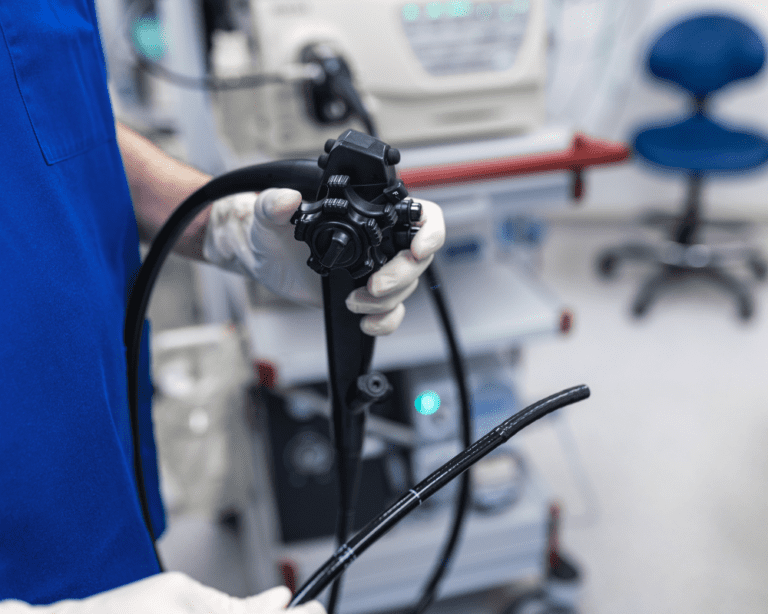
Diagnosing Crohn’s before modern tools was like trying to guess dinner ingredients blindfolded. You might get it right eventually, but not before wrongly blaming something else. From tuberculosis to stress, Crohn’s was frequently mislabelled — partly because its symptoms mimic a dozen other gastrointestinal conditions. The tools got better (endoscopies, blood tests, even inflatable balloons), but the psychological challenge remained: how do you confidently identify something that mimics half the ailments in the medical textbook?
Blood tests are another handy tool in the Crohn’s diagnosis toolbox. Doctors can check for certain markers, like C-reactive protein or erythrocyte sedimentation rate, which can signal inflammation.
And here’s a quirky tidbit: some doctors have even used a humble balloon to diagnose Crohn’s. Yes, you heard that right. They inflate a balloon inside your intestine to see how it responds. It’s like a high-stakes game of “Guess the Reaction.”
Who Was Burrill Crohn and Why Does the Disease Carry His Name
Poor Burrill Crohn. He didn’t even want his name tangled up in digestive dysfunction. Yet history gave him credit — or perhaps blame — for a condition he described alongside Ginzburg and Oppenheimer. When Crohn’s disease was first discovered in 1932, the trio identified inflammation of the terminal ileum as something distinct from tuberculosis or ulcerative colitis. It was Burrill Crohn whose name stuck, thanks to alphabetical luck and a landmark paper.
Dr. Crohn was a brilliant mind with a keen interest in understanding the human digestive system. His groundbreaking work on Crohn’s disease not only helped identify it but also paved the way for future research and treatments.
In his own words, Dr. Crohn once said, “This new entity, which I propose to call ‘terminal ileitis,’ may be confused with other diseases of the intestinal tract and may be far more common than the records now indicate.” Little did he know that his words would echo through the decades, changing the lives of countless individuals who would be diagnosed with Crohn’s.
Why Crohn’s Was Misdiagnosed for Decades
Crohn’s wasn’t merely late to the medical party — it spent decades being mistaken for someone else. For years, doctors lumped it together with tuberculosis or ulcerative colitis, often treating it with the medical equivalent of “turn it off and on again” (read: remove part of the intestine and hope for the best).
Here’s where psychology meets pathology. Humans — especially doctors — have a habit called confirmation bias. Once you’ve seen something that looks like TB, you tend to keep seeing TB. Our brains are pattern-recognition machines with a tendency to shout “AHA!” far too early in the process. Crohn’s didn’t fit neatly into the known patterns, so it kept slipping through diagnostic cracks.
Add to that a dollop of naming bias. You see, once Burrill Crohn’s name entered the record books, it focused attention on the symptoms he described — inflammation of the terminal ileum. But Crohn’s can pop up anywhere along the digestive tract. By giving it a specific name, the medical community ironically constrained its own understanding of the condition.
This is what behavioural economists call framing effects. What we call something changes how we treat it. Label a condition as psychological, and people assume it’s “all in your head.” Call it autoimmune, and suddenly it’s taken more seriously. Language doesn’t just describe reality — it shapes it.
And finally, let’s not forget the role of discomfort. Not just the physical kind — but the cultural variety. Nobody in polite society wanted to talk about diarrhoea, bloating, or intestinal strictures at the dinner table. So Crohn’s remained hidden in plain sight — socially invisible, clinically slippery.
It wasn’t until patient voices grew louder and medical tools got sharper that Crohn’s began to gain the respect (and research funding) it deserved. And that’s a lesson worth remembering: sometimes the hardest thing to diagnose isn’t the illness — it’s the assumptions surrounding it.
How Common Is Crohn’s Disease in the UK and What the Numbers Reveal
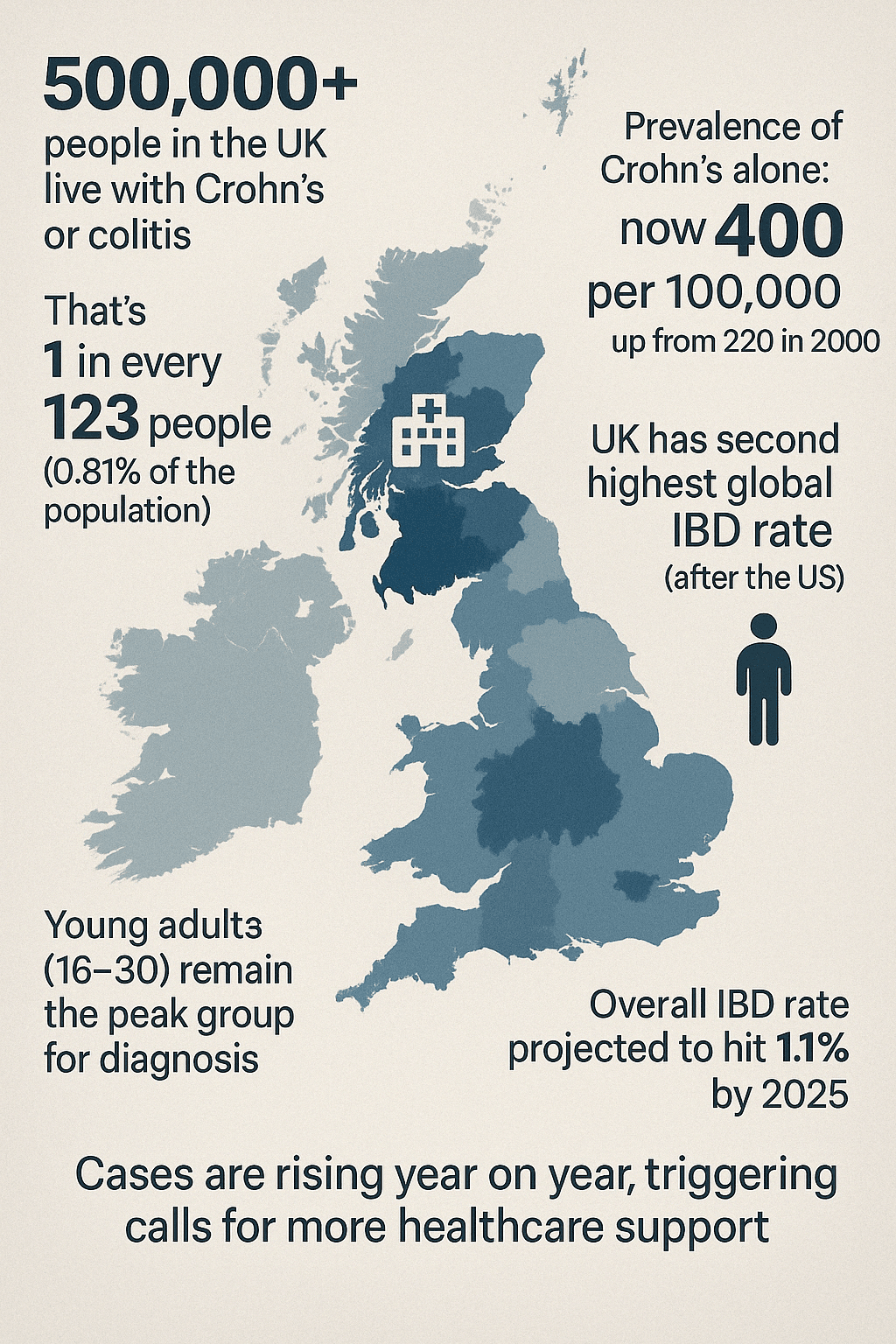
The numbers for Crohn’s alone have climbed dramatically — rising from 220 to 400 cases per 100,000 people between 2000 and 2017. And it doesn’t stop there. Projections suggest IBD will affect 1.1% of the UK population by 20251, pushing it closer to a national health crisis than a niche diagnosis.
To put it bluntly, Crohn’s disease statistics in the UK now place us among the top countries globally — second only to the United States2. And while that’s not exactly a podium you want to stand on, it should at least raise eyebrows in public health circles.
What’s more, the condition continues to rise most rapidly among young adults3, raising uncomfortable questions about environmental triggers, diet, and whether anyone in their 20s can ever trust their stomach again. The call for greater awareness, early diagnosis, and better support services has never been louder — or more justified.
Quick Stats on Crohn’s in the UK
- 500,000+ people in the UK live with Crohn’s or colitis
- That’s 1 in every 123 people (0.81% of the population)
- Prevalence of Crohn’s alone: now 400 per 100,000, up from 220 in 2000
- UK has second highest global IBD rate (after the US)
- Young adults (16–30) remain the peak group for diagnosis
- Overall IBD rate projected to hit 1.1% by 2025
- Cases are rising year on year, triggering calls for more healthcare support
Crohn’s Remains a Medical Riddle Wrapped in Gut Reactions
The history of Crohn’s disease reveals a fundamental truth: medicine is often less about facts and more about persistence, personality, and pattern recognition. Burrill Crohn wasn’t just medically sharp — he was curious enough to say “What if we’re wrong?” And frankly, more doctors could benefit from that kind of intellectual humility.
As Dr. Crohn himself showed us, curiosity and determination, can lead to groundbreaking discoveries. So, whether you’re battling Crohn’s, supporting a loved one through their journey, or just curious about what’s happening in your gut, remember that knowledge is power.
As you navigate the twists and turns of life with Crohn’s, keep in mind that you’re part of a community that’s growing and learning every day. And while we’re still unraveling the mystery, together, we’re getting closer to understanding and managing this uninvited guest in our digestive party.
So here’s to fewer surprise sprints to the loo, and more nights when pizza is just pizza — not a ticking time bomb.
And as the great Dr. Burrill B. Crohn once said, “The more I know, the more I realise how much I don’t know.” In the world of Crohn’s, we’re all on a journey of discovery, one step at a time.
Note: Always consult with a healthcare professional for the most current information on Crohn’s disease.
Common Questions on the History of Crohn’s Disease
Crohn’s disease was first formally described in 1932 by Dr. Burrill Crohn and his colleagues, though symptoms had been misattributed for decades prior.
Burrill Crohn was a gastroenterologist who helped define the condition now known as Crohn’s disease. Ironically, he didn’t want it named after him.
Its symptoms mimicked tuberculosis and ulcerative colitis, and for decades, diagnostic tools weren’t precise enough to distinguish it.
Around 115,000 people in the UK have Crohn’s disease, with high diagnosis rates among young adults aged 16 to 30.
When Crohn’s disease was first discovered in 1932, Burrill Crohn and his colleagues observed symptoms that mimicked tuberculosis but were clearly distinct — a breakthrough that redefined gastrointestinal medicine.