If you or someone close to you is seeking Crohn’s disease treatment NHS support, it can feel like trying to solve a puzzle with three pieces missing. The system is there to help, yet it is not always obvious where to begin. Here is a clear route through the NHS so you can move from symptoms to a plan, with less guesswork and fewer dead ends.
Getting a Diagnosis on the NHS
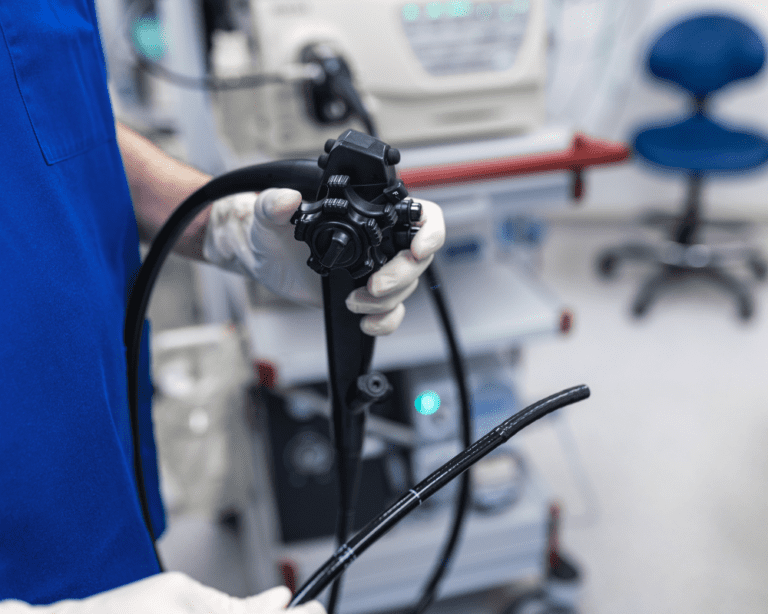
Getting a Crohn’s disease diagnosis can sometimes feel like untangling Christmas lights, frustrating, time-consuming, but worth the effort. Since symptoms can mimic IBS, coeliac disease or infections, persistence helps. See your GP if you have abdominal pain, diarrhoea, weight loss or rectal bleeding. Ask about the GP referral process for inflammatory bowel disease and tests such as bloods, faecal calprotectin, endoscopy and colonoscopy, or imaging. If needed you will be referred to gastroenterology. If you are searching online, terms like Crohn’s disease diagnosis NHS can help you find reliable pages.

Finding a Specialist
Your GP refers you to an NHS gastroenterologist Crohn’s disease clinic. That specialist will assess symptoms, order tests, and agree an IBD treatment plan. You can use NHS website tools to compare hospitals and services near you. You can also manage bookings via the NHS e-Referral Service.
Useful search terms if you get stuck
- NHS Crohn’s disease referral
- NHS gastroenterologist Crohn’s disease
- NHS e-Referral Service Crohn’s
- Crohn’s disease diagnosis NHS
Overcoming Waiting Times in the NHS
Waiting can be the hardest part. NHS waiting times Crohn’s disease vary by area, but a few small tactics can shorten the treatment timeline.
- Ask to be added to cancellation slots and be flexible with dates.
- Use the e-Referral portal to check other hospitals with shorter lists.
- Call the appointments team or clinic secretary for late openings.
- Ask the IBD nurse about triage if symptoms worsen, they can escalate.
- Consider a private gastroenterologist Crohn’s disease consultation for a faster assessment, then continue care on the NHS.
Think of it like catching an earlier train. You still reach the same destination, you simply swap to the platform that is moving.
Crohn’s disease treatment NHS explained
After diagnosis, your gastroenterologist and IBD nurse will shape your plan around disease location, severity and your goals. Treatments include steroid therapy for flare-up management, immunomodulators, and biologic therapy. Monitoring is part of the picture, from bloods to faecal calprotectin and occasional scopes, to check response and maintain remission. Some medicines need NHS Crohn’s medication approval, usually guided by NICE, and your team will handle prescription approval. When symptoms persist or complications develop, NHS Crohn’s surgery options are discussed with a colorectal surgeon.
Questions to ask in clinic
- What does my IBD treatment plan aim to achieve in the next 3 to 6 months
- Which tests track progress, for example endoscopy and colonoscopy or faecal calprotectin
- What are the likely side effects and safety checks for this medicine
- What happens if I flare again, and who do I contact

Living Well with Crohn’s Disease Through the NHS
Care is not only tablets and scopes. Ask for a referral to an NHS dietitian. They can help you spot dietary triggers, build a safe food diary, and support nutrition during flares and remission. In some directories you may see NHS dietician for Crohn’s disease, it refers to the same specialist.
For emotional health, ask about NHS mental health support Crohn’s through NHS Talking Therapies, which offers counselling and cognitive behavioural therapy. Many IBD teams also link to local support groups where people speak frankly about the everyday stuff, from fatigue to fear of long queues when you need a loo.
If symptoms limit work or study, an occupational therapist can suggest practical changes and equipment so daily tasks take less energy.
Managing Healthcare Costs
NHS care is free at the point of use, yet there can be extras like travel and parking. If you have regular prescriptions, consider an NHS Prescription Prepayment Certificate, which can be cheaper than paying each time. Ask about hospital travel cost schemes if you receive certain benefits.
Patient Rights and Advocacy Resources
You have rights in the NHS, including involvement in decisions and access to a second opinion. If you hit barriers with an NHS Crohn’s disease referral or appointments, contact the hospital PALS team. Charities such as Crohn’s & Colitis UK offer guides, helplines and template letters that make self-advocacy easier.
Advocating for Yourself Within the NHS
Bring a short summary to each appointment, top symptoms, any new medicines, and one clear priority for the visit. Keep copies of clinic letters and test results. Apps like Patient Access help you track prescriptions and messages.
Prepare questions in advance, for example how this drug helps remission, what monitoring is planned, and what to do if side effects appear. If a plan does not suit you, say so. Good care is a conversation, not a monologue.
If progress stalls, ask about alternatives, such as switching biologic therapy, reviewing steroid use, or seeing surgery to discuss options. You can have a brief private gastroenterologist Crohn’s disease review for speed, then continue within the NHS if you prefer.
Conclusion
Accessing care for Crohn’s in the UK takes patience, but small, smart actions help, from using the e-Referral portal to leaning on IBD nurses and dietitians. With a clear plan and the right support, you can move from firefighting flares to protecting remission.
Remember This blog post is intended for informational purposes only and should not be construed as medical advice. Always consult your doctor to discuss your individual situation and the best course of treatment for you. Do not start or stop medications without speaking to a doctor. Do not change your diet without speaking to your doctor or a healthcare professional.
Common Questions About Crohn’s and the NHS
Start with your GP. They can order initial tests and refer you to gastroenterology for assessment and scopes if needed.
Options include steroids, immunomodulators, biologic therapy and surgery. Your team will tailor an IBD treatment plan.
Ask for cancellation slots and check other hospitals on e-Referral. Contact the IBD nurse if symptoms escalate.
Usually yes. Your GP or specialist requests endoscopy and colonoscopy as part of diagnosis or monitoring.
Your team follows NICE guidance and local pathways. Some drugs need prior approval before prescribing.
Yes, many people do. You can then continue Crohn’s disease treatment NHS care if you prefer.
Ask for an NHS dietitian and NHS Talking Therapies. Both support daily life alongside medical care.