Finding promising treatments for Crohn’s disease can feel like trying to fix a leaky tap during a power cut. You know what you need, you just wish someone would hand you the right tools. The good news, backed by solid research, is that new options are arriving, and many are already helping people feel better and stay better for longer.
The importance of early diagnosis in Crohn’s disease
Early diagnosis of Crohn’s disease helps improve treatment results and reduce complications. Spotting symptoms early means you can start treatment before inflammation causes lasting damage. Common early signs include persistent diarrhoea, abdominal pain, weight loss, and fatigue.
If you or someone close to you experiences these symptoms, speak to a healthcare professional. Diagnosis often involves blood and stool tests, imaging, and sometimes an endoscopy. There is no single test that confirms Crohn’s disease, yet this combination helps rule out other conditions and identify inflammation in the digestive tract.
Why act early? Delays can lead to fistulas, abscesses, and bowel obstructions that might need surgery later. Earlier diagnosis gives access to more options, including less invasive medicines and lifestyle changes, so you can manage the condition more effectively.
Researchers are also advancing personalised medicine, often called precision medicine for Crohn’s disease. This approach aims to match the right treatment to the right person, which may improve remission rates and reduce side effects over time.
Promising treatments for Crohn’s disease biologic therapies
Biologic therapies for Crohn’s disease target specific parts of the immune response that drive inflammation. Many people with moderate to severe IBD benefit from these medicines, especially when other treatments have not helped enough. Well-known options include Infliximab and Adalimumab, with new biologic treatments for Crohn’s disease arriving through ongoing trials.
These medicines can reduce flare-ups and support remission. Your medical team will consider your health history, current symptoms, and test results before recommending a biologic therapy or a small molecule alternative.
Diet and lifestyle changes for Crohn’s disease management
Medication is only part of the picture. Diet changes for Crohn’s disease and practical lifestyle changes for Crohn’s disease can support gut health and daily energy. There is no single diet for everyone, though some approaches help many people.
During flare-ups, a low-residue diet can reduce fibre and give the bowel a rest. Examples include white rice, lean proteins, and well-cooked vegetables. Between flares, some people find an anti-inflammatory diet for Crohn’s disease helpful, focusing on foods rich in omega-3 fatty acids, a variety of fruits and vegetables that they tolerate, herbs like turmeric, and gentle cooking methods.
Probiotics and fermented foods such as yoghurt, kefir, and sauerkraut may support gut health. Tolerance varies. A registered dietitian can help you test changes safely and tailor a plan to your symptoms and goals.
Stress management, movement, and sleep matter as much as menus. Short walks, yoga, or mindfulness can lower stress, which may influence symptoms. Think of it as tuning the whole system, not just the digestive part.
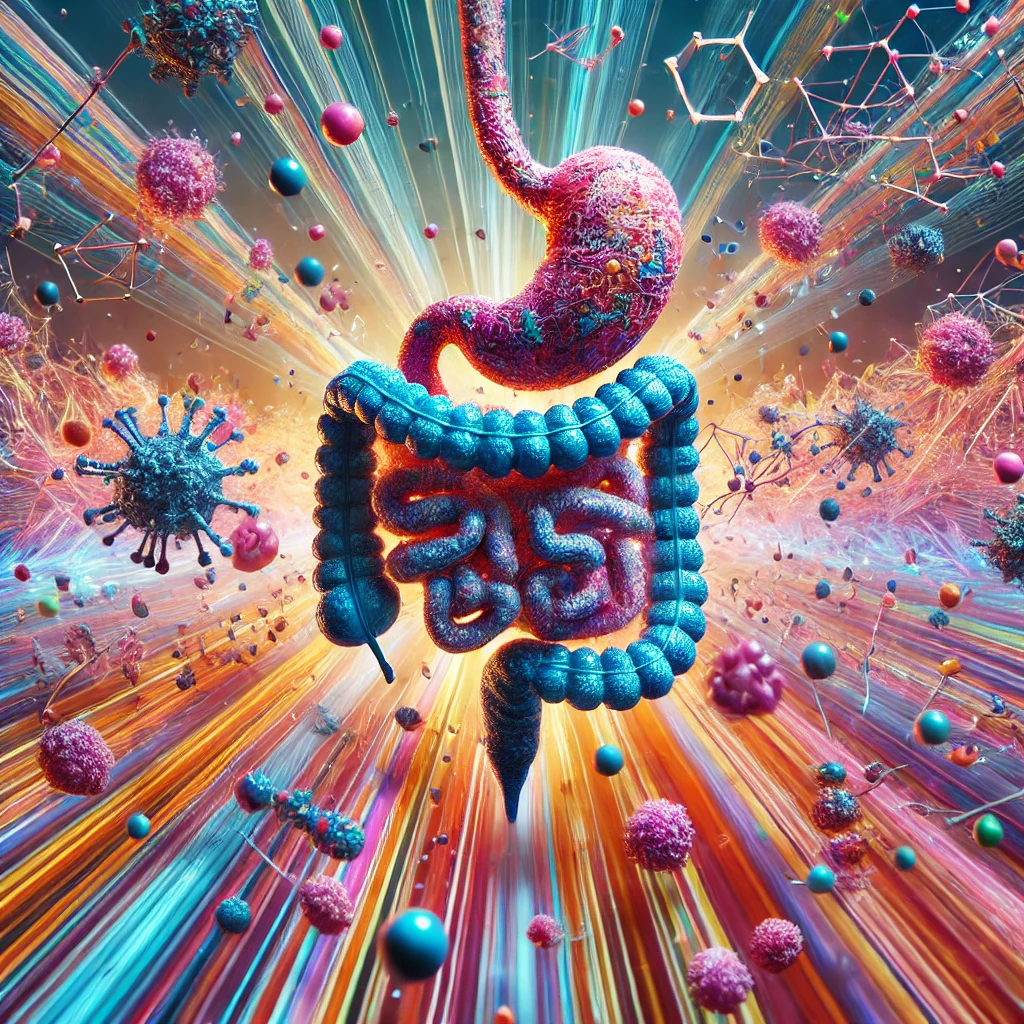
Faecal microbiota transplantation rebalancing gut health
Faecal microbiota transplantation for Crohn’s disease is being studied as a way to restore a healthier gut ecosystem. It transfers carefully screened donor bacteria to the recipient with the aim of improving balance in the microbiome. Early studies are mixed but encouraging in some groups, especially when FMT is part of a wider plan that includes diet and medicine. Talk to your gastroenterology team if you want to understand current evidence and availability in the UK.
Exploring cutting edge clinical trials for Crohn’s disease
Clinical trials for Crohn’s disease bring new options to people who have tried standard therapies. Current research includes biologics, small molecule drugs, and faecal microbiota transplantation. For example, Risankizumab targets a specific inflammatory pathway and has helped some people who did not respond to other treatments. Studies of oral small molecules such as Filgotinib aim to offer convenient, at home dosing.
If you are curious about trials, ask your gastroenterologist about eligibility, safety, and practical details. Taking part is a personal decision that weighs potential benefits against risks and time commitments.
Mental health and coping with Crohn’s
Crohn’s disease affects mood, confidence, and social life, not only the bowel. Anxiety and low mood are common, particularly during flare-ups or after hospital stays. Talking therapies, peer support, and simple breathing or grounding techniques can lighten the load. Small rituals help, like packing a go bag for clinic days or using a symptom note on your phone to track patterns without overthinking them.
Share what you need with people you trust. Clear, honest explanations can turn awkward moments into practical support, which makes daily life easier.
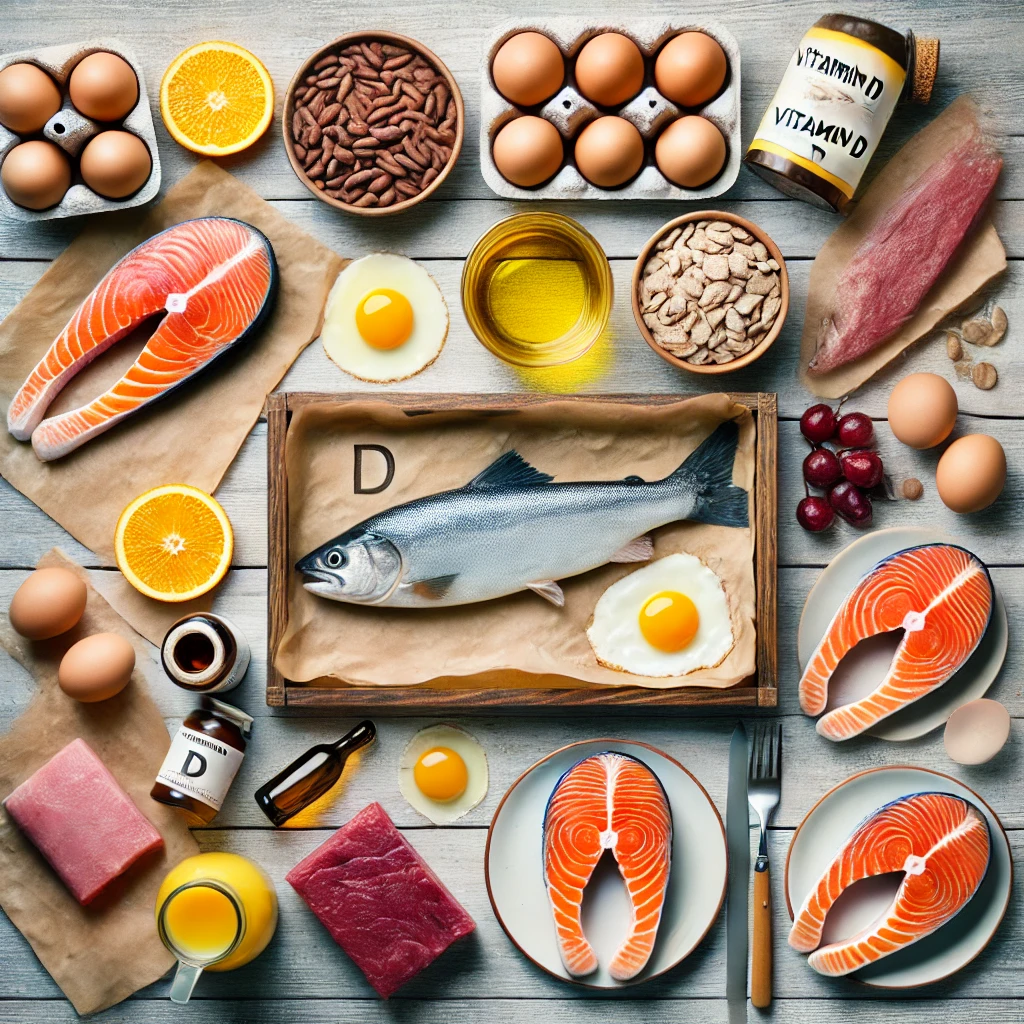
Vitamin D and Crohn’s management
Research suggests vitamin D status may be linked with inflammation and immune function in Crohn’s disease. Low levels are common. Testing and individual advice from your doctor can guide safe use of food sources or supplements, especially if you spend limited time outdoors or avoid certain foods.
Innovations shaping Crohn’s treatments
Alongside established medicines, researchers are studying approaches that could change long term care. Precision medicine for Crohn’s disease aims to predict who will respond to which therapy, reducing trial and error. Gene and cell based strategies are being explored to modulate immune activity. Stem cell therapy is under investigation for healing damaged tissue in selected cases.
The gut microbiome and Crohn’s disease remain a priority in research. Better mapping of microbes may lead to targeted diets, probiotics, or next generation treatments that restore balance more reliably.
Practical notes on surgery and monitoring
Some people still need surgery for strictures, fistulas, or other complications. Surgery can improve quality of life, yet it is not a cure, so ongoing medical care and monitoring remain important. Regular check ins, blood tests, and endoscopy when recommended help track inflammation and support earlier action if symptoms change.
How to use this information in real life
Bring this page to your next appointment and highlight the parts that fit your situation. Ask about managing Crohn’s disease symptoms day to day, and whether any new biologic treatments for Crohn’s disease or small molecule options might suit you. If you are interested in research, ask about nearby studies and what taking part involves.
Medical information notice Remember, this blog post is intended for informational purposes only and should not be construed as medical advice. Always consult with your doctor to discuss your individual situation and determine the best course of treatment for you. Do not start or stop medications without speaking to a doctor. Do not change your diet without speaking to your doctor or a healthcare professional.